
I call it the menopause narrative, and it goes like this:
“Women are safeguarded from heart disease until menopause when their risk escalates dramatically. You have this short timeframe to start estrogen or else you're screwed.”
I've been aware of flaws in this narrative for some time, and recent studies have served as a reminder. And I hope you’ll agree that this is good news.
Quick note: this does not apply to women who go through menopause early or experience surgical menopause before the natural age of menopause.
The science behind the narrative
A quick review for those who are new or just need a refresher from my heart health post on my blog.
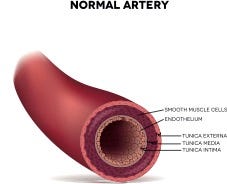
One of the key functions of both estrogen and progesterone, and their receptors, is that they help stimulate nitric oxide (NO) production in the vascular endothelium. This is the layer of cells that line blood vessels, which are critical to vascular health and function.
This is summarized in this 2018 review in Heart and Circulatory Physiology:
Generally, E2 [estradiol] exposure in women increases vascular relaxation and endothelial-dependent vasodilation, increasing blood flow in numerous vascular beds. NO bioavailability can also be impacted by oxidative stress, and it is well known that estrogens have antioxidant capabilities.
In short, having a healthy endothelium plays a central role in vascular tone, insulin sensitivity, blood flow, and blood pressure regulation.
This is important because you need a healthy endothelium to keep plaque from forming on the vessel wall. And dysfunction of the endothelium is thought to be the precursor to heart disease.
So, when women eventually experience a decline in sex hormones, they lose this protective effect of sex hormones on the endothelium.
Hormone therapy can help restore this to a certain extent, but this effect lessens with age. This is especially true when it’s started after 60 or over 10 years from menopause.
Older women can experience a lot of fear when they hear they missed out on taking hormones at the right time. But there’s much more to the story.
Read: Heart health for women over 40 comes down to this
The downplayed role of aging
When women take hormone therapy closer to menopause, they have less risk, which is true. But there’s a piece missing which was shown in a 2017 study in Scientific Reports.
To separate the effects of aging and menopause, researchers conducted an in vitro analysis of the effects of estrogen in both large and small arteries in mice and women.
In the present study, we have sought to determine the contributions of age or menopause on arterial function and estrogenic responsiveness in vitro.
The researchers chose two different age groups for mice (24 and 29 months) to reflect ages 69 to 80. For the women, they separated them into age groups: 30-39, 40-49, 50-59, 60-75.
Aging had no effect on the acute response to estrogen. Yet age negatively affects the maximum ability for arteries to relax. These impairments started at age 50 but ramped up by age 60.
These weakened responses to estrogen were because of the beginning stages of endothelial dysfunction. The age group that responded the best to estrogen was the 30–39-year-olds.
The researchers conclude that both chronological age and menopause affect the vasodilatory effects of 17B estradiol. In particular, aging affected endothelial dysfunction before estrogen responsiveness in those small resistance arteries. Here’s what they had to say:
We, therefore, propose that age-related changes in arterial endothelial function and/or stiffness are prominent factors, and not just menopausal status per se, leading to impaired estrogenic actions in arteries from post-menopausal women.
Don’t estrogen receptors decline with age?
It’s speculated that it’s the years from menopause that blunts estrogenic vasodilation due to declining expression of estrogen receptors.
Yet in the study just mentioned, there was no difference in ER expression in resistance arteries for women over six years from menopause.
A comprehensive study released in June by Lisa Mosconi et al showed an increase in ER density in the brain as women moved further away from menopause.
We need to remember the body still makes estrogen but in much smaller amounts, so perhaps the body increases receptors to compensate.
Who knows, but the key is that our estrogen receptors may not shrivel up if we don’t go on hormone therapy.
Why does heart disease spike at menopause?
It’s true that heart disease risk rises in women over 50, and menopause plays a role. My view is that menopause acts like a tipping point for women.
For example, the effects of aging are gradual and not as noticeable. Then hormones shift and eventually decline over a shorter period.
Estrogen loses its vasodilator effect, similar to a team losing one of its star players. If the rest of the team has been stepping up, the loss may not be so bad. But if they haven’t, they may need some time to adjust.
Another explanation comes from a study in BMJ that showed when separating cardiac events out, the risk of coronary heart disease is less in women over 55.
It has also been proposed that the leveled risk of men and women around 50 is due to decreases to cardiac events in males with age.
Either way, risk goes up after 50, but it’s not all menopause’s fault.
A recent study gives us hope
I wrote this post because I found a study thinking, “It’s about time.”
In this small, double-blind randomized control study, researchers examined the effect of nitrate-rich beetroot juice on arterial function in menopausal women.
Disease-free early menopausal (<6 years) and late menopausal (>6 years) women drank daily beetroot juice rich in nitrates (400mg) or without nitrates for seven days.
To test vasodilation, they used flow-mediated dilation (FMD) but also tested endothelial injury, which is a temporary period of blood flow restriction and repair.
This is a way to test the resilience of the endothelium. In a previous study by the same research team, 100 minutes after a single dose of nitrate-beetroot juice, early menopausal women showed improved resilience to endothelial injury.
The investigators tested arterial function 24 hours after the last seven-day dose. They found FMD increased by 2% in both groups of women but had no effect on the response to endothelial injury.
To give you an idea, FMD percent is typically around 8-10% premenopause and drops to 4-6% post-menopause, so a 2% increase is great.
This shows that beetroot juice had a positive effect on vasodilation in both early and late postmenopause women. But after 24 hours, the resilience piece declines, and the authors speculate women may need to keep drinking the juice daily to get those benefits.
The goal: a healthy and happy endothelium
This is not about bashing hormone therapy which is a lifesaver for some women, Instead, I’m seeking to understand how Aging Pause influences endothelial health and what women can do regardless of their age.
In one study of young women with and without insulin resistance, estrogen did not dilate small blood vessels in those with insulin resistance (IR), but it did in the women without IR. And these women were in their 20s!
The great news is that there are a multitude of ways to boost endothelial health including nitrates in beetroot juice, as already stated, which isn’t affected by age.
Of course, the work being done at University Colorado Boulder on inspiratory resistance strength training and blood vessel health, including how midlife omen respond to exercise.
And for women who do well on hormone therapy, keeping your endothelium healthy is key. I’d love to see more studies on what can increase women’s response to estrogen.
Thankfully, estrogen is not the only vasodilator and antioxidant because its effect declines with age. And we need to let midlife women know, especially older women who feel like they missed the boat.
Key takeaways
Women are told that menopause (alone) increases the risk of heart disease and estrogen is the solution that needs to be started close to menopause—This narrative is incomplete as research also shows aging changes to endothelial health affect the ability of estrogen to dilate blood vessels, not just time from menopause.
One theory is that estrogen receptors decline with time from menopause, but newer evidence challenges this.
Both aging and menopause affect heart health, and a new study with beetroot juice shows that high nitrates produce a good blood vessel dilation response in both early and late post-menopausal women.
Whether or not on hormone therapy, preventing or reversing endothelial dysfunction is crucial because estrogen’s effect lessens with time.
The new menopause midlife narrative
I’d like to change this narrative that menopause is solely to blame for heart health issues in midlife women. How does this sound?
The risk of heart disease increases for women during midlife due to aging, and menopause accelerates this risk. Whether or not women choose hormone therapy, preventing or reversing endothelial dysfunction is crucial.
I got in touch with Beet-it Sport, which is the juice used in the study, and they are offering a 10% discount with the code Maryann10. This product has been used in over 300 studies!






I am one of those women aged 60 who feels like they may have missed out health wise and lots of other ways by not being able to go on HRT. Your article has helped me see this in a different light. Thank you.
Informative helpful information. Menopause is highly vulnerable time when so little information is available while doctors (those younger) seem to have little interest in learning about it.