A roundup of at-risk menopause micronutrients
Why isn't anybody telling midlife women their micronutrients needs change as they transition through menopause?
One of the biggest surprises I’ve found in researching midlife health is how sex hormones affect nutrition status. My theory is that when we are fertile – and have regular cycles – our hormones work to ensure adequate nutrition status.
It makes sense, right? A body that is trying to get pregnant is going to differ from one that isn’t. Now that doesn’t mean we can’t become deficient or run low on nutrients when we have cycles. In fact, if key nutrients and calories dip too low, we don’t have enough body fat, or are so stressed out, we simply won’t ovulate.
But our hormones do extra lifting behind the scenes that we may not even be aware of. For instance, both women of childbearing age (WCBA) and women of menopause age (WMENO) have shortfalls in calcium, magnesium and vitamins A, C, D and E. According to this research:
Substantial percentages of WCBA and WMENO are not meeting recommendations for multiple nutrients, whereas supplement usage partially fills nutrient gaps
Yet despite this, we really don’t feel the effects of certain nutrient shortfalls until our hormones change. Aging matters too, but we’ll get to that in another post.
So even though I’ve written about these nutrients before, I wanted to do a roundup of the key micronutrients every midlife woman needs to stay on top of. Let’s start with two that affect brain health.
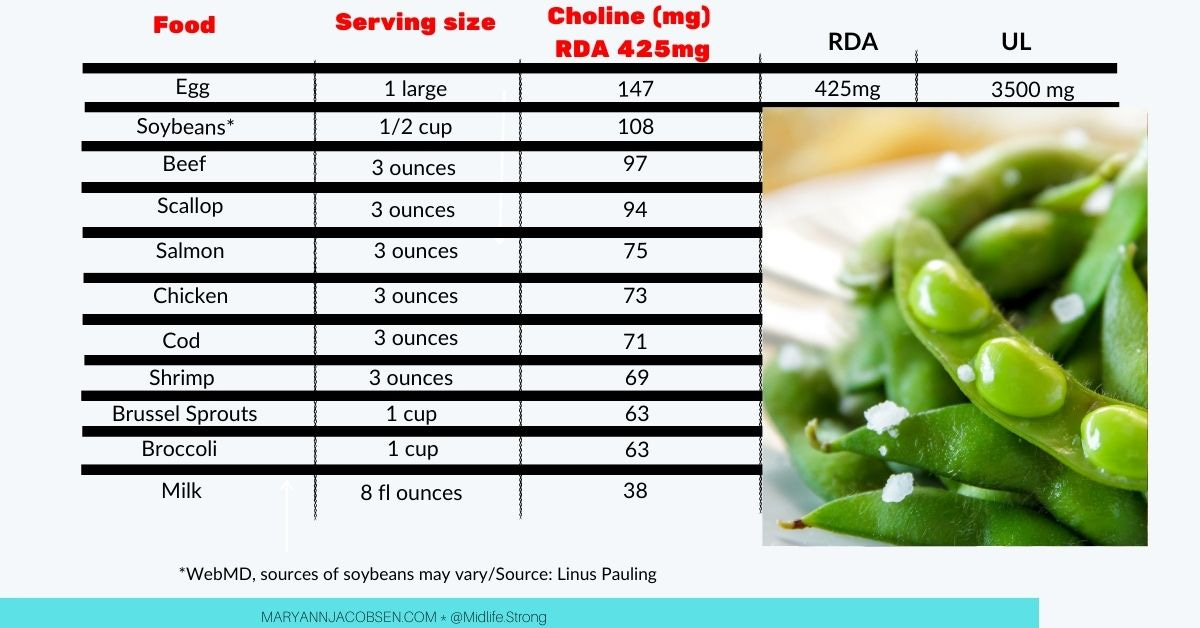
Choline
Choline is necessary for making phosphatidylcholine and acetylcholine, a neurotransmitter involved in memory. Researchers have linked deficiency of choline to memory dysfunction.
Estrogen is thought to help stimulate phosphatidylethanolamineN-methyltransferase(PEMT), an enzyme that can help increase choline in the body. This means estrogen helps to make choline even when intakes are low.
For instance, fifty-six adults (26 men, 16 premenopausal women and15 postmenopausal women) were fed a choline-deficient diet (50mg) for 42 days. When deprived of choline, 77% men and 80% of the postmenopausal women showed signs of organ dysfunction (a sign of choline deficiency) while only 44% of the premenopausal women did.
I’m just going to add that this research was done in 2007 and we’ve done little on helping midlife women get adequate choline!
According to a recent review:
The promoter region of PEMT contains an estrogen response element (ERE) and its mRNA and activity are dramatically upregulated in response to estrogen exposure, buffering premenopausal women and postmenopausal women taking estrogen replacement therapy from the organ dysfunction associated with consuming a choline-deficient diet
In the Framingham Cohort, high choline intake was linked to better cognitive performance and smaller white matter hyperintensities volume (WMHV), found to be neuroprotective.
Most women only get 294mg choline and not the recommended 425mg. So, at midlife–a time our bodies make less — we need to be especially mindful of this nutrient. Supplements are tricky because they may increase a substance known to increase heart disease although we need more research. Citicoline is the most safe and well studied one that has been shown to aid memory.
Research suggests adequate choline intake helps maintain the bioavailability of DHA. Without choline, the DHA we get through diets or supplements may not be as effective. That’s because phosphatidylcholine (PC), phospholipids that utilize choline, helps transport DHA into the body.
And DHA just happens to be our next nutrient.
DHA
As we get older, long-chain fatty acids DHA (and EPA to a lesser extent) play a key role in a woman’s brain health. That’s because brain volume declines with age, and DHA levels decline as well.
Estrogen aids the conversion of ALA to DHA and EPA for women which matters during menopause. According to one review on the subject:
Young women convert the plant omega-3 FA, ALA, to EPA and DHA with a greater efficiency than do young men. Endogenous estrogen seems to stimulate the biosynthesis of long-chain omega-3 FAs from common dietary precursors, presumably via stimulation of the δ-5 and δ-6 desaturases, the rate limiting enzymes in PUFA biosynthesis
Even though our brains change with age and hormonal shifts, there’s so much we can do to boost brain health and DHA and EPA are part of that.
In the Framingham cohort, people in the top quartile for DHA experienced a 47% lower risk of dementia. And according to a study in Neurology, post-menopausal women with a higher omega-3 index had larger brain volume and hippocampal volume than those with lower omega-3 index. This difference in brain volume equated to about 2 years of brain aging.
According to a 2021 review in Aging Research Reviews, “The greatest bulk of evidence indicates that greater hippocampal volume is associated with higher levels of omega-3.”
Most of us fall short on consuming two fatty fish portions per week, which comes out to 500mg DHA per day. But research shows that even when we consume fish two-times per week may not be enough to keep our omega-3 index levels >8%, which is recommended.
That’s why I recommend getting tested at a place like Omega Quant. Getting tested helped me increased my omega-3 index from just over 6 to 8.5%.
Magnesium
Magnesium is involved in more than 300 biochemical reactions in the body. Some experts think it's actually 600!
It plays many roles in the body, from brain function and mood to helping maintain strong bones. It’s also important for maintaining muscle and nervous system function, cardiac electrical properties, vascular health, and helping regulate insulin and glucose metabolism.
Magnesium is a major shortfall nutrient in women's diets. The RDA is 320mg for midlife women, yet 64% do not reach 265mg/day with an average intake about 246mg.
Long-term insufficient magnesium is linked to higher levels of free radicals and chronic diseases. Complicating matters is evidence showing that may lead to lower levels of magnesium.
In animal studies, ovariectomized rats have reduced serum magnesium, which causes an inflammatory response. One review states that “Estrogen enhances Mg reabsorption in the kidney and absorption in the gut by stimulating TRPM6 expression.”
In fact, magnesium fluctuates with the menstrual cycle as estrogen ebbs and flows. And lower magnesium in the second half of the cycle has been implicated in premenstrual syndrome (PMS). Plus, taking magnesium helps reduce PMS symptoms.
Magnesium likely plays a role in menopause symptoms too, but the research is not as clear.
Complicating things even more, many medications decrease magnesium absorption, including diuretics and proton pump inhibitors. And stress may also increase the need for magnesium.
We may be quick to supplement but I always suggest checking diet first and considering increasing magnesium in the diet. I get over 400mg from my diet (I’m a nut freak!) and only take it when I think I need it.
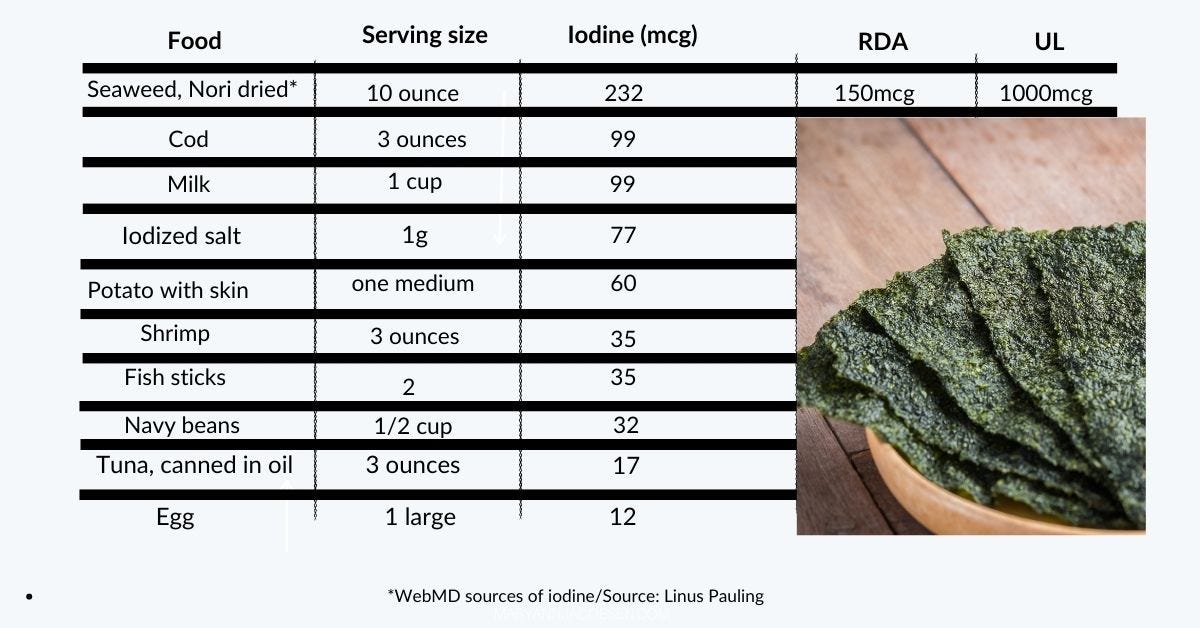
Iodine
As women transition through menopause, risk of thyroid function dysfunction increases. That’s because estrogen has both direct and indirect on the thyroid. Iodine matters because it’s needed to make thyroid hormone.
Although estrogen's effect on iodine uptake is uncertain, it's important to aim for 150mcg of iodine to ensure proper thyroid support.
There is also evidence that magnesium deficiency can lead to decreased uptake of iodine in thyroid cells, another at-risk nutrient we already mentioned.
Iodine is also important for heart, breast, and bone health. And studies suggest people with lower urinary iodine are at increased risk of heart disease. And when thyroid function gets whacky, it can increase blood pressure and blood lipids – something that takes women by surprise around menopause.
I found an interesting study that iodine status correlates with symptoms of perimenopause and menopause. And iodine deficiency was more commonly seen in subjects with hypertension and who were postmenopausal.
Iodine intake has been on the decline for years now, with urinary iodine decreasing from 320mcg/L in 1970 to 145mcg/L in 2000. Iodine is not in many foods, which is why iodized salt was introduced many moons ago.
It’s also in dairy products, fish, seaweed, and iodized salt. With many giving up dairy, no longer using iodized salt, and that most of us don’t eat fish daily, it’s a potential problem.
But Iodine does not work alone. It needs its pal selenium.
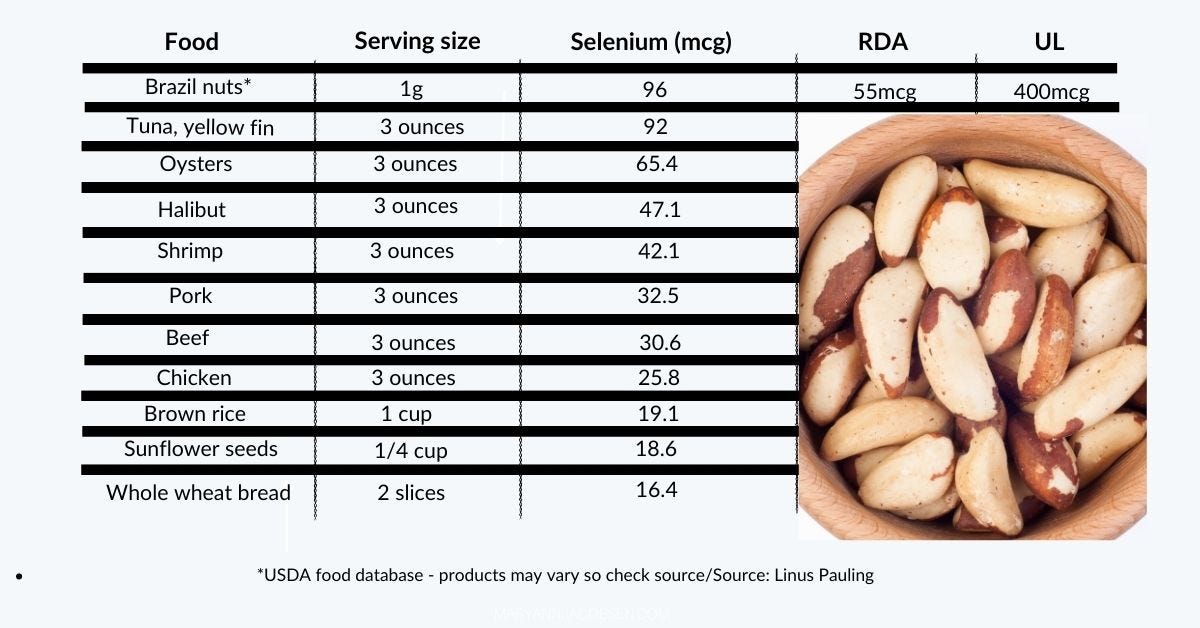
Selenium
Research is unravelling the role selenium plays in thyroid health. A study in the Journal of Clinical Endocrinology found the risk of thyroid dysfunction 69% higher in low-selenium areas.
High levels of iodine may have negative effects on thyroid but selenium is protective, meaning we need to be sure we’re getting both iodine and selenium.
“Selenium is well-known to protect the thyroid,” said researcher Margaret Rayman, in this Endocrine Web article. “The importance is that we have shown that low selenium is associated with an increased risk of thyroid disease.”
And that’s not all, estrogen may also play a role in selenium status according to animal studies. In rats, estrogen increased selenium status as measured by selenium concentration and GPx activity in plasma, liver, brain, and red blood cells. The researchers conclude:
Preliminary findings from our laboratory strongly support the likelihood of a relationship between selenium and estrogen availability.
Selenium has also been found to play a role in the prevention of cancer, boosting the immune system, and lessening anxiety and depression. The RDA is set at 55mcg although some studies show 100mcg may be optimal for midlife women. We need more research to know for sure.
What can we do? Increase selenium in your diet and consider a multi that includes selenium (this is what I take). I do not recommend selenium supplementation at high levels unless directed by a health professional as its benefits are U shaped.
Vitamin D
We’ve known for a long time that vitamin D helps the body maintain the right balance of calcium and phosphorus. If you don't have enough vitamin D, your body won't be able to deposit enough calcium into your bones to maintain their strength and health..
But vitamin D isn’t just about bone health anymore. Over the last two decades, researchers have found many conditions associated with low vitamin D levels, from heart disease to diabetes to autoimmune diseases.
The reason for this has to do with another discovery: most body cells have a vitamin D receptor. This means vitamin D plays a role in many of the body’s functions.
Two things change during menopause. First, we have an increase in body fat, which can increase our needs of vitamin D. And second, was something tested back in 1986!
Twenty premenopausal women had their vitamin D levels checked during their cycle. When estrogen decreased, so did vitamin D. And when it increased, so did vitamin D.
A recent large prospective cohort found that vitamin D supplementation resulted in a 40% reduced risk of dementia. And get this. The effect was stronger in women! In fact, when separated out, women who supplemented with vitamin D had a 49% reduced risk.
This potential relationship makes it even more important to have vitamin D levels monitored during midlife. That way we can adjust the doses of supplementation since diet will almost always fall short!
We need more research
Of course, I had to dig to find this research, and we certainly need more to know for sure how menopause affects these nutrients.
But that’s the problem I will keep mentioning again and again. We need to understand how the needs of women change as they age and go through menopause.
In the old days, I’d just pop some D and was good to go. Now, I’m careful to meet my needs for these at-risk nutrients and in my book l will walk women through each step of the way. I believe testing is best so if you haven’t yet grab my biomarker guide by signing up for this newsletter!
Let me know your questions in the comments!







I love this! It helps to explain all my cravings and all my imbalances SO WELL! I’m going to make a handy dandy list to stick on the fridge. You wouldn’t happen to have a pdf like that would you?