When to exercise, The Mediterranean Diet (without wine?), and two new biomarkers
June Midlife Roundup [2024]

“Simply by replacing your morning coffee with green tea, you can lose up to 87%....
Of the little joy you had in your life.”
This is a social media gem, I tell you.
It reminds me of the delicate balance between health and pleasure. Something I think about often.
This theme came up as I gathered information for this round up. If we take something away (or change something) in the name of health, but are less happy from it, does that harm health?
There’s a lot of fear producing health information out there for midlife women. When you look carefully, it’s not always so clear cut. And when you dig deep, there are often more questions than answers.
Let’s touch on two health-related messages and break them down a bit, so we can more clearly see what they are all about.
Is there an optimal time to exercise?
When I saw the NY Times headline “Should you exercise in the morning or evening?” I was eager to see what it had to say.
According to an Australian study mentioned in the article, middle-aged adults with BMIs over 30 who exercised in the evening had a 28% lower risk of death.
Despite being interesting, it’s just one of many studies with conflicting outcomes.
“It’s not settled,” said Juleen Zierath in the piece, a physiologist at the Karolinska Institute in Sweden. “It’s an emerging area of research. We haven’t done all the experiments. We’re learning a lot every month.
Other studies show that morning exercise is better for heart health and may help sleep. I peaked at the comments, and everyone seemed to think the same thing.
The best time to exercise is the time that works best for you. I like early morning, but I also switch it up, because I also like to write early.
Perhaps being open and trying different things is key until you land at what feels right.
Competitive athletes are a different story because they are always looking for an advantage. According to the article, small studies suggest that nighttime might be more favorable for performance because of rising body temperature.
Another potential advantage is evening workouts may aid in promoting insulin sensitivity. As I layout in my intermittent fasting post, we are less efficient at glucose metabolism in the evening compared to the morning.
But we don’t have to do formal exercise, we can simply go for a walk after dinner. Studies have shown that these walk help improve blood sugar and insulin response.
There are so many times and ways to move our bodies. Let’s avoid rigid standards.
While many of these studies are fascinating, none of them is definitive. For one thing, most are simply showing a correlation between exercise times and health benefits, not identifying them as the cause. - NY Times, May, 4, 2024
Removing wine from the Mediterranean diet?
While scrolling on social media, I came across a familiar, fearful post. One person predicted that in the future, alcohol consumption will be viewed similarly to smoking.
In short: alcohol is the new smoking.
This anti-drinking for health sentiment is everywhere. Although excess alcohol is no doubt harmful, I feel these messages leave out big chunks of information. And don’t acknowledge that giving up drinking may not be right for everyone.
It ignores the large body of observational data showing moderate drinking may help reduce reduced cardiovascular disease and mortality. In fact, one of the key elements of the Mediterranean diet is moderate wine consumption.
The PREDIMED is one of few randomized control studies showing that the Mediterranean diet decreases heart disease risk by 30% over 5 years. There is a 14-item adherence questionnaire of which drinking a glass of wine daily is one of them.
Wine has been a strong risk-lowering factor of the Mediterranean diet. Researchers estimate that removing wine could decrease the benefits by 12-24%.
However, because of concerns about the health effects of alcohol, The European Research Council is funding a large randomized controlled trial (RCT) beginning this month.
The four-year study involves 10,000 people, with half receiving counseling on the Mediterranean diet with wine, and the other half receiving counseling on the diet with alcohol abstinence.
As I mentioned in my big post on alcohol, the pattern of drinking and the type of alcohol may be key. The Mediterranean way of drinking spreads drinks out throughout the week, includes red polyphenol-rich wine, and does it while enjoying a nutritious meal.
The modeling studies like the Global Burden of Disease in both 2016 and 2020 did not include the pattern of drinking, which stated that there is no safe amount of alcohol (which was later revised slightly due to benefits of small amounts of alcohol in those over 40).
Of course, individually giving up (or cutting back) drinking can help people improve their health. But continuing to drink moderately may be right for others.
We have been lacking large, randomized control studies on drinking, so I’m jazzed about this news. What do you think?
Updated Biomarker Guide
I just updated my Biomarker Guide for midlife women, adding biomarkers: uric acid and lipoprotein a.
I dug into uric acid after a friend told me her levels were high. I never gave much thought to it before besides risk for gout. Elevated uric acid levels, especially in women, have been found to increase the risk of heart disease.
Uric acid is a byproduct of purine metabolism. When it increases in the body, it can crystalize in joints, which is why high levels cause gout flares. High levels also disrupt The One Health Principle, depleting the body of nitric oxide.
Uric acid increases as women transition to menopause. Estrogen helps to clear it from the system, so as estrogen levels decline, it can become elevated.
This is another area that researchers have not studied thoroughly, as high uric acid is also linked to joint pain and osteoarthritis.
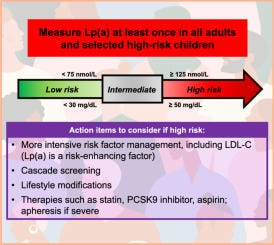
The second test is Lipoprotein a pronounced “lipoprotein little a,” Lp(a). It is a genetically inherited lipoprotein responsible for carrying cholesterol and triglycerides in the body.
Lp(a) is a strong independent risk factor for cardiovascular disease that is not modifiable. Current guidelines from the National Lipid Association recommend testing Lp(a) once in adulthood to assess cardiovascular risk.
Researchers are testing medications to lower Lp(a) but as of now, it is only used to assess risk. It can help you and your healthcare provider decide on whether to add a treatment or just assess your genetic risk for heart disease.
Levels below 75 nmol/L (30 mg/dL) are low risk, while levels above 125 nmol/L (50 mg/dL) are high risk. Despite its significance, awareness is low; a study across six centers in a California health system from 2012 to 2021 found that only 0.3% of patients were tested.
I’m going to ask my doctor to check mine at my next physical in the fall. Here are some related articles on it:
Future Lp(a) Treatment Options by Dr. Paddy Barrett
High Lp(a) Warrents Intervention (results of a new study) by Peter Attia
American Heart Association details about lipoproten (a)
A little time off
I’ll be taking a break next week, so there won’t be any new posts. If I decide to post, it will be a thread or something simple.
As you likely know by now, simple is hard for me, but sometimes I can do it.
My youngest graduated 8th grade and I officially have two high schoolers, but only for one year. I’m going to spend some extended time with my family.
As always, thanks for being part of this community. It truly means a lot.