
It’s November. Can you believe it? I’m in California and we just turned our clocks back. I love gaining an hour on the day we change the clocks. But now it means it will get darker earlier, which I don’t love so much.
I wanted to let you know of a webinar I’m giving tomorrow at Medfit entitled “Menopause or Micronutrient Deficiency?” It’s free and if you can’t make it, they send you the recording.
Medfit also has other educational webinars that you might want to check out.
New study on HRT and Alzheimer’s
A new systematic review and meta analysis on HRT and its relationship with dementia and Alzheimer’s has been in the news. There was an article on CNN entitled “Sweet sport for HRT may reduce dementia risk by nearly a third.”
The paper included 6 RCTS and 45 observational reports, which includes almost 800,000 women. Randomized control studies in women over 65 found increased risk with estrogen/progesterone therapy (EPT) but neutral effects with estrogen only. Pooled data showed reduced risk with estrogen only (32%) and a nonsignificant decrease in EPT (22.5%)
The largest effect (32% reduction) was for women on estrogen only. When a woman is on estrogen only, she doesn’t have a uterus and therefore doesn’t need progesterone. The Menopause Society recommends women who've had a hysterectomy or surgery that puts them in menopause early take hormones at least until the natural age of menopause (52) unless there are contradictions.
“These observations suggest that, while the risk of dementia increases with surgical menopause, it may be reduced when estrogen therapy is initiated within the ‘critical window’ and continued for an extended period of time.”
The main theory why estrogen only may be more protective is that progesterone competes for estrogen receptors. This research does not differentiate synthetic progestins from micronized progesterone, with the latter being more commonly prescribed these days.
Progestins are not the same structure of progesterone that our body makes, like micronized progesterone. See Hot Flash Inc’s article on why the difference matters.
I’m not blown away with this research. My gut tells me that we will never get answers on dementia risk and hormone therapy. No doubt it's safe and better to start before age 60 or withing 10 years after menopause, and it's especially important for early and/or surgical menopause. Yet, I think we overlook the other strategies, apart from hormones, that can help lower the risk of dementia.
Other ways to lower dementia risk
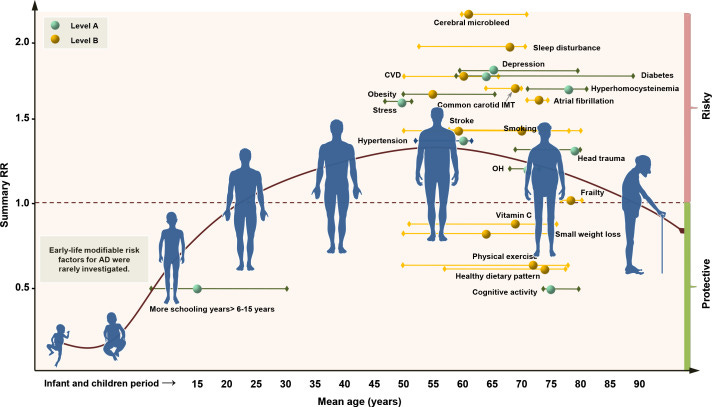
In 2020, researchers published a first-of-its-kind comprehensive, large-scale systematic review with 243 observational studies and 153 RCTs to find effects for lowering dementia risk. The researchers provided a grading for the strength of the evidence, as shown below.
Level A (strong evidence): education, cognitive activity, high body mass index in late life, hyperhomocysteinaemia, depression, stress, diabetes, head trauma, hypertension in midlife and orthostatic hypotension
Level B: obesity in midlife, weight loss in late life, physical exercise, smoking, sleep, cerebrovascular disease, frailty, atrial fibrillation and vitamin C
You read that right, hyperhomocysteinaimia is in there (a hot topic for me—read more about it here). Homocysteine also goes up with menopause. Just another reason to check it and be sure you’re getting enough B vitamins to keep it <10. These researchers are also surprised.
“It is striking that, apart from one meta-analysis, the PAR estimates suggest that from 12% to 31% of cases of dementia or AD could be prevented by lowering tHcy.”
Let’s not forget the emerging data on omega-3s and choline. A recent study using longitudinal data on omega-3 DHA and EPA and dementia found that taking omega-3 supplements reduce dementia risk by 64% and dietary intake by 20%. And I discuss the exciting research on choline and Alzheimer’s on Instagram.
What is SOOO interesting is that choline, omega-3 and B vitamins work synergistically to lower homocysteine and improve brain health. B vitamins have been found to be more effective in improving cognition in those with a higher omega-3 index. Perhaps this is all too new to make it to systemic reviews.
For me, the estrogen-can-lower dementia risk is simply not as interesting as all the other things we can do. And I’m excited to see where the research goes.
Other midlife health news
I often cite an article from psychologist and life span development expert Margie Lachman in 2015 where she calls for more midlife-targeted research.
She mentions how there are no journals or associations dedicated to midlife, like there are with other life stages. Yet in that same year, 2015, the Women’s Midlife Health Journal was born. And I just found out the publication is closing.
What?
They state that since they started the journal that other journals have stepped up:
“Over the past decade, as scientific knowledge has increased, documenting the importance of the midlife for healthy aging, menopause journals have expanded their scope and aging journals have expanded their breadth. As multiple excellent venues are now available to publish work on midlife health, we have decided to cease publication of this journal.”
But why can’t we have a journal dedicated to midlife health? Why do we need to piggyback on other journals?
I’m more and more convinced that the health needs of midlife women are very different from the general population. Just general “eat healthy and exercise” is not adequate. Many women experience health woes and never find actual answers. And while hormone therapy is safe and great, it’s not the only answer.
I’ll be talking more about this, especially in terms of exercise.
Midlife Vaginas
I had a friend growing up who always called vaginas Va JJ. There seems to be a stigma talking about our Va JJ or vaginas even as we get older. I found a string of articles on the subject of midlife vaginas.
On Instagram, I saw a new study in the JAMA network about how vaginal estrogen doesn’t affect cancer mortality in breast cancer survivors. Younger women who get breast cancer may go into menopause early due to treatments. Regardless, many cancer survivors who have symptoms, including vaginal dryness, and have been told not to take estrogen.
Yet vaginal estrogen has minimal absorption and does not carry the same risks as systemic hormones. This study summarized on Medscape may help put both women and health practitioners at ease.
Of course, while I was at Medscape, I found another article about the real risks entitled “Vaginal Dryness Can Be Fatal. No, Really.” In it, Dr. Rachel Rubin details the risks associated with changes to the vagina during the menopause transition, called Genitourinary Syndrome of Menopause (GSM).
“It turns out that all of the genital and urinary symptoms from menopause just get worse over time. The bladder, the urethra, and the vagina have lots of hormone receptors, including estrogen and testosterone. When the body no longer makes those hormones, the system doesn't work very well, and genital and urinary symptoms occur that just get worse over time without treatment. Unlike hot flashes, which tend to go away, GSM does not.”
This can increase the risk of infections like UTIs. I recently read that 55% of postmenopausal women have an uptick in UTIs. And this can cause many problems over time.
And that gets me to a post I read on Lady Parts here on Substack speculating about how the Golden Bachelor’s wife Toni died. It seems it was from a bacterial infection that led to sepsis. Could it be due to a UTI? Did she have GSM and not get treated? Here’s what Deborah Copaken had to say:
“Call me crazy, but I would go so far as to say that not naming the cause of Toni’s seemingly sudden bacterial infection was a massive missed opportunity for a teachable moment in front of millions of middle-aged women and their partners. Why, on a network show celebrating and showcasing elder sex, would those in command of such decisions choose not to explain the all-too-common origins a bacterial infection that is so often precipitated by the elder sex they are cheekily promoting?”
As we go through menopause, we must take action to care for our vaginas. Some doctors still think vaginal estrogen has the same risk as systemic hormone therapy, when it clearly doesn’t. And if you can’t take estrogen, there are other therapies like DHEA you can talk to your doctor about.
Well, that’s enough to think about for this November round-up. I hope your November is off to a great start!




Thanks for mentioning my story! :)