Stand up for women: make ferritin screening a standard
The case for universal ferritin screening

When I heard the about the White House Initiative for Women’s Health research last November, I immediately thought about iron deficiency without anemia. I wrote an opinion piece that I pitched twice, and it sat on my computer. Hearing that things are under way, spurred me to not only publish the piece here but to start a Change.org petition. This issue should have been taken care of decades ago but here we sit with no IDWA screening guidelines and women – and their future children – suffering. Please consider signing my petition and sharing this post and/or my petition with others. Thank you!
The White House announced its new initiative for women's research on November 13th, 2023, led by first lady Jill Biden. The project is well under way with Biden recently announcing 100 million in research. "We will build a health care system that puts women and their lived experience at its center,” she said. “Where no woman or girl has to hear that, 'oh, it's all in your head’ or ‘it’s just stress.’”
If we are serious about building a women-centric healthcare system, there’s one action that will provide the most bang for women’s buck: universal ferritin screening. I’m referring to the public health epidemic of iron deficiency without anemia (IDWA), which occurs mostly in women due to iron loss during the menstrual cycle and those who become pregnant.
Although current guidelines call for anemia screening, IDWA is three times more common. By the time doctors diagnose a woman with iron deficiency anemia, defined as a hemoglobin less than 12 g/dL, she is in the third and final stage of iron depletion. Although inflammation can cause elevated levels of ferritin, it is the gold standard for diagnosing iron deficiency. It reveals the amount of stored iron which works like an iron savings account for your body–when it runs low, you’re in trouble.
I should know because it happened to me. I had two children right before I turned 40, followed with regular, ample periods for 10 years, and I’m a runner. This combination of risk factors–of which no health professional asked about - led me to iron deficiency anemia right at 50. I thought my heart palpitations, swallowing problems, intermittent high heart, driving anxiety, periodic dizziness, and fragmented sleep were due to changing hormones. Nope, it was a lack of iron. When I looked back at my labs over the years, I could not find one ferritin. Not one!
Once I was anemic, my doctors then checked my ferritin, which was 10 mcg/L. Research suggests that symptoms of fatigue can occur when ferritin dips below 50 mcg/L, much higher than the World Health Organization (WHO) cutoff of 15 mcg/L and the National Institute of Health cutoff of 30 mcg/L. No wonder my 40s were an exhausting decade. But I was astonished with how "not new" this problem was.
In the 1950s, bone marrow staining became the gold standard for diagnosing iron deficiency since declining or absent bone marrow iron negatively affects erythropoiesis (making red blood cells). Studies found that not only were women more likely to be iron deficient, but 2/3rds of young US women had low iron stores while half had hemoglobin levels in the 5 percentile of men. A ferritin as high as 50 mcg/l resulted in absent bone marrow in 50% of women, suggesting that only levels as high as 100 mcg/L could ensure iron repletion in healthy young women.
This begs the question: how many women throughout recent history have suffered from IDWA? Let’s consider present day. If we take the lowest cutoff for ferritin from WHO, 17% of young women are deficient. If you increase that to a ferritin of 25 mcg/L, it jumps to 40%. And when the cutoff is 50 mcg/L, nearly 80% would be deficient. In a Spanish population of 18-93-year-old’s, using a cutoff of 30 mcg/L, nearly 60% of menstruating women were deficient, which decreased at menopausal age. But still 20-30% remained at low levels even after menopause. Yet on a population basis we’re doing nothing to identify these women.
“For years my ferritin levels have been below 15, yet 3 different doctors told me that I don’t need supplemental iron,” wrote one woman, responding to a blog post I wrote on ferritin. And another chimed in with doctors not even making the connection with her symptoms: “I have been going to the doctor for years complaining of tiredness, shortness of breath, achy muscles, headaches, etc. – not once were my iron levels checked.”
IDWA is not just about symptoms, it’s a health issue. Although best known for its function in making hemoglobin to transport oxygen, iron is part of 180 biochemical reactions. These include thyroid hormone synthesis, immune function, DNA synthesis, neurotransmitter synthesis and cellular respiration in the muscles, heart, and energy metabolism. The same way a declining savings account forces people to spend less, the body pulls back on these functions to conserve iron for oxygen transport. In short: it prevents anemia at all costs.
In fact, many diseases linked to iron deficiency have a high female to male ratio including thyroid dysfunction (8:1), fibromyalgia (8-9:1), chronic fatigue (4:1), IBS (2-2.5:1), depression (2:1), restless legs (2:1), long covid (1.6:1) and allergies (1.4/1). For instance, in the aforementioned Spanish population, thyroid hormones decreased right along with ferritin levels. In pregnant women, iron deficiency increases the risk of overt and subclinical clinical hypothyroidism. Women with iron deficiency are 66% more likely to experience allergies and patients with restless legs, and a ferritin less than 75mcg/L, show improvement with iron supplementation. Of course, iron deficiency alone does not cause these issues, but evidence suggests it plays a contributing role.
Then there’s the known cost of iron deficiency on both pregnancy and childhood health outcomes, which include but are not limited to higher risk of cognitive impairment and behavioral problems in children. Can you believe there are still no ferritin screening guidelines for pregnant women? Iron status may even affect a woman’s ability to conceive. Women with a ferritin less than 30 mcg/L were more likely to experience unexplained infertility (33%) compared to controls (11%) according to a 2023 study.
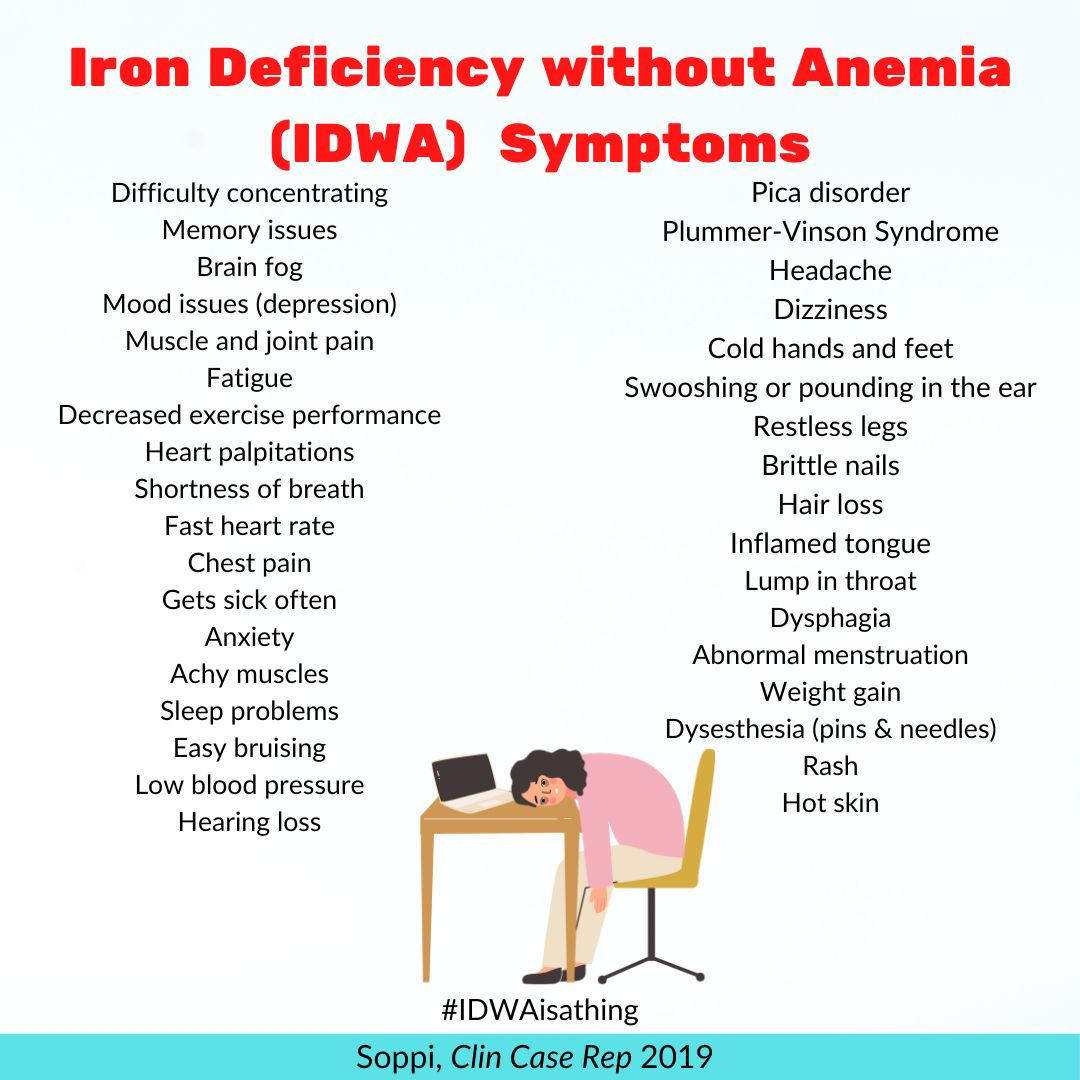
“During my 30-year career as an internist with a special interest in thyroid diseases and hematology, I have met hundreds of patients, mainly menstruating females, who seek advice because of prolonged (1–25 years) fatigue, brain fog, muscle and joint pains, weight gain, headache, dyspnea, palpitations, sometimes associated with sleep disturbances, arrhythmia, lump in the throat or difficulty in swallowing, and restless legs,” writes Esa Soppi, MD, PhD, adjunct professor in medicine from Finland who first wrote about the challenges of treating IDWA in the 2018 journal Clinical Case Reports. “At least 30% of patients with a diagnosis of chronic fatigue syndrome (CFS), ADHD (especially children when there is a history iron deficiency of the mother) and long covid have a wrong diagnosis since iron deficiency causes all of their symptoms.”
In addition to lower quality life and health of women, mismanaging iron deficiency is a strain on the medical system. A significant number of women (46.6%) receive psychotherapy, medical therapy (think heart tests for palpitations) and medications for symptoms later to discover iron deficiency caused them. Making matters worse is the longer a woman has been iron deficient, the harder it is to treat. “A small proportion of patients (1–5%) do not seem to respond to iron at all, not even after several years of follow-up,” writes Soppi in a 2022 piece in the European Society of Medicine. “Usually the cause lies in a protracted duration of iron deficiency of 15–25 years or more.”
No wonder countless researchers and health organizations have called for universal ferritin screening throughout the years, including most recently the International Federation of Gynecology and Obstetrics. In the summer of 2023, researchers from the University of Western Australia not only called for ferritin screening, but detailed what it should look like.
“Though there are available guidelines for diagnosing an iron deficiency in otherwise healthy reproductive aged women, the exact ferritin thresholds used are commonly inconsistent between both laboratories and practices,” said lead researcher Beth MacLean, when asked why there aren’t ferritin screening guidelines for women. “The absence of iron deficiency screening guidelines for women are likely a result of these inconsistencies in the definition of iron deficiency in this cohort coupled with an under-appreciation of the impact that an iron deficiency can have on a woman’s wellbeing.”
The researchers recommend ferritin screening at least every 5 years, starting three years after menstruation until menopause, and more frequently in those at high risk. They suggest 30 mcg/L as the point to offer iron supplementation with daily iron (65mg elemental) which can be given every other day, especially in cases of poor tolerance. Three months after starting supplementation, ferritin should be higher than 30 mcg/L and be continued until levels reach 50 mcg/L. IV iron should be considered if a patient fails to reach an initial ferritin of 30 mcg/L. This differs from traditional treatments that give high iron, multiple times a day, for short time periods, and no ferritin goal or long-term follow-up.
During my 30-year career as an internist with a special interest in thyroid diseases and hematology, I have met hundreds of patients, mainly menstruating females, who seek advice because of prolonged (1–25 years) fatigue, brain fog, muscle and joint pains, weight gain, headache, dyspnea, palpitations, sometimes associated with sleep disturbances, arrhythmia, lump in the throat or difficulty in swallowing, and restless legs. -Esa Soppi, MD, PhD
Soppi encourages clinicians to be aware of presenting symptoms of IDWA. “If symptoms are in accordance with iron deficiency, the patient should be considered iron deficient at least up to a serum ferritin concentration of 100 mcg/L, or even much higher, if the patient has an inflammatory condition, kidney disease or fatty liver,” he recommends. For instance, 10-20% of doctor visits have fatigue as a primary driver. Before referring women to a cardiologist or therapist, doctors should always investigate and consider iron supplementation when appropriate. This is especially important for midlife women who, like I did, tolerate symptoms assuming they are due to perimenopause.
Let’s unpack this for a minute. Adopting universal ferritin screening could prevent or reduce certain health conditions, improve the quality of life of women, ensure better iron status at the beginning of pregnancy, and save money and healthcare resources. What are we waiting for?
The White House Initiative on Women’s Health Research must address this this healthcare gender gap that harms the health of women around the globe. The time has come for universal ferritin screening in menstruating women.
Please sign my Change.org petition demanding comprehensive ferritin checks for women.




My ferritin lab result is 39.3 ng/mL. Not measured in mcg/mL. What is difference between ng vs mcg?