Is the stomach to blame for midlife digestive issues?
Unveiling the stomach's importance in digestive function–and overall health
About 10 years ago, I started experiencing these strange stomachaches. I would usually experience this piercing pain when I was stressed. I’d overextend myself to find “oh no, my stomach is doing that thing again.”
Laying down for 5 minutes did the trick. But it probably is not a coincidence that this occurred in my 40s, a time when stomachs become vulnerable.
I’m not alone. Every day a midlife woman experiences a new digestive issue, whether that’s stomachaches, bloating, reflux, nausea, or intolerance to a previously tolerated food or drink.
Most of these digestive issues originate in the stomach. I wanted to talk more about the stomach in my 21-day gut health challenge, but decided it was too much.
Somewhere along the journey to researching midlife, I realized that a working, functional stomach is an overlooked and vital part of maintaining health. It’s so important that I see it as the heart of the GI tract.
The functioning stomach’s Fab 4
What do I mean when I say the stomach is the heart of the GI tract? The stomach's job is to store the food you eat temporarily, break down that food, kill pathogens, and move food out into the small intestine.
Instead of pumping blood, it’s pumping food. It’s not only pumping food but also transforming it. In fact, our stomach is already gearing up to do its job as we chew and swallow food. The food then travels down the esophagus and empties into the stomach.
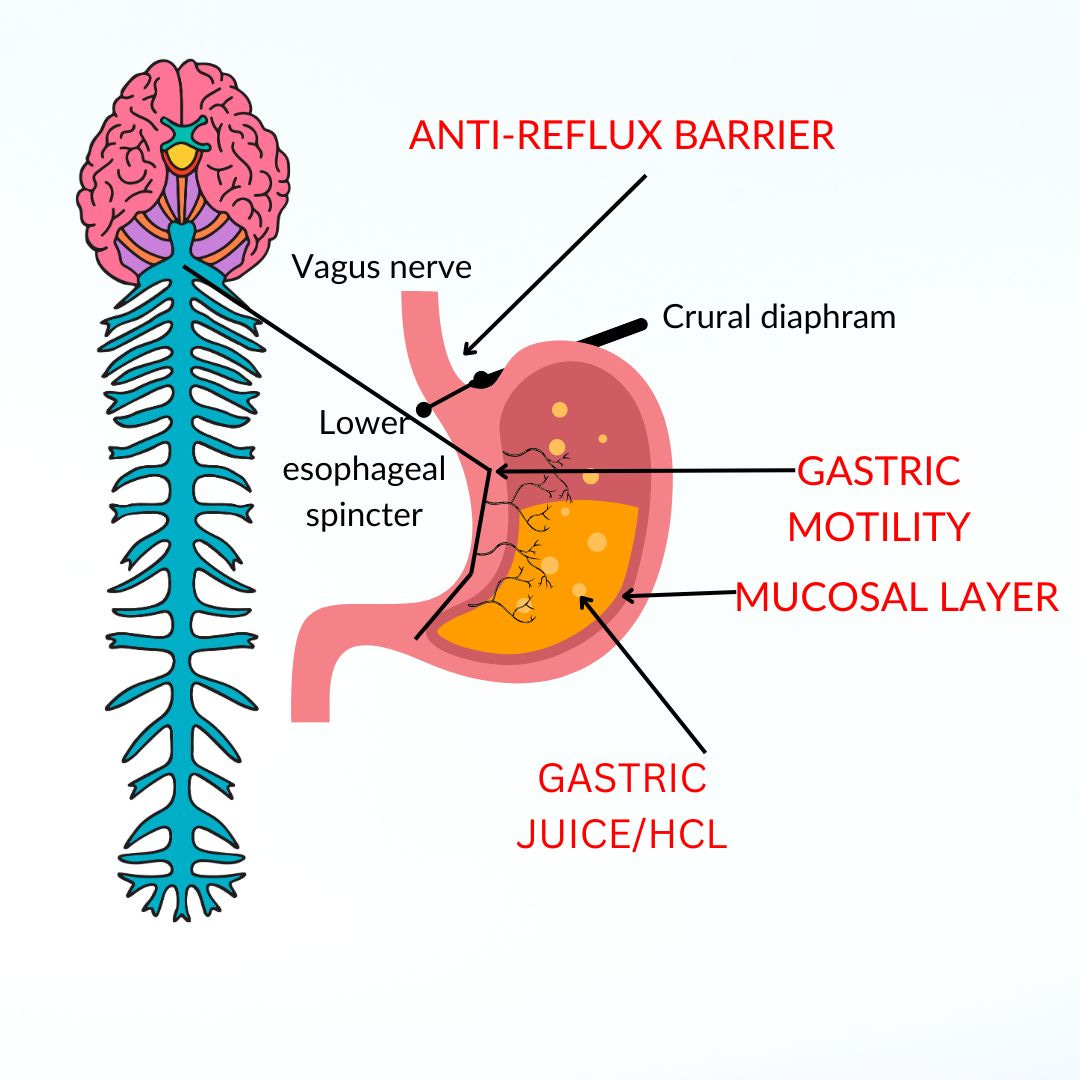
The esophageal sphincter and the crural diaphragm overlap to create the gastro-esophageal (anti-reflux) barrier. The anti-reflux barrier helps keep food in the stomach, the way heart valves shut to keep blood moving in the right direction.
The stomach’s protector is the gastric mucosa, which is the layer of mucus that lines the stomach. It helps move and moisten chyme (mixture of food and digestive enzymes), while creating a barrier, keeping the stomach from digesting itself.
Parietal cells of the stomach secrete gastric juice, which contains hydrochloric acid (HCL) and digestive enzymes. HCL is one million times stronger than the acidity of blood or saliva, capable of making stringy meat the texture of soup through the process of digestion.
As chyme moves from the upper to lower stomach, a low Ph (1-2) induces the release of pepsin, an enzyme that helps digest protein. A low pH is necessary to convert nitrates found in vegetables into nitric oxide (NO), the magical midlife molecule. NO helps maintain gastric blood flow, which strengthens the gastric mucosal barrier.
The last component of the stomach is gastric motility, which at first lets food sit by relaxing smooth muscles, and then gently contracts those muscles to move food along its way. This is done with the help of nerve fibers, which we’ll get into in a bit.
The Fab 4 includes the anti-reflux barrier, mucosal layer, gastric juice, including HCL, and gastric motility shown below. Before we get into what can go wrong, there’s one more vitally important thing an optimally functional stomach does.
The stomach and micronutrients
When the Fab 4 are working in harmony, it creates the ideal environment for micronutrients to get absorbed in the intestine.
First is through the complete breakdown of food, and as one review states, “releasing nutrients from their organic complexes.” One example is how HCL cleaves vitamin B12 from food and intrinsic factor attaches to it to usher it along.
Second is making micronutrients bioavailable. For instance, HCL turns ferric iron into an absorbable ferrous state, with the help of vitamin C.
An acidic environment in the stomach also helps break down calcium salts to soluble calcium chloride, which aids absorption in the proximal small intestine. Other micronutrients that rely on a healthy, functioning stomach include vitamin C, magnesium, and possibly vitamin D.
A functioning stomach also helps to maintain a healthy gut microbiome by killing pathogenic bacteria and fully breaking down food. This also decreases the risk of intestinal illness, such as food poisoning.
This often-forgotten link between the stomach and micronutrients may have a relevant impact on a huge amount of people. -Carabotti et al., Nutrients, 2021, p. 12
Declining stomach function is one key reason micronutrient absorption declines with age. So, let’s take the Fab 4 and look at them individually, to see what can go wrong with the heart of the GI tract during Aging Pause.
Declining Anti-Reflux Barrier function
Midlife women often reach for antacids more frequently because of heartburn. This is when the anti-reflux barrier transiently relaxes, allowing food to come back up to the esophagus, resulting in a burning sensation.
At midlife, gastro-intestinal reflux disease (GERD)–defined as two or more of these reflux episodes a week — increases in women, reaching about 15%.
After a meal, the contents of the stomach move from the proximal stomach to the distal stomach. Yet with reflux, there appears to be larger “acid pockets” that escape the buffering effect of meals in the upper stomach.
The acid pocket is a physiologically normal phenomenon; however, patients with GERD have larger acid pockets than healthy individuals. - Arguero, 2024 Apr;21(4):282-293.
Researchers used to think that it was the acid that damaged the esophagus, but emerging research shows that the release of acid and bile causes an inflammatory reaction.
We do not completely understand the reasons for GERD increasing with age, but many factors, including lifestyle, can play a role.
A recent large population-based study in women and men aged 35-65 linked increased risk with smoking, alcohol, inactivity, high intake of sweets and desserts, low intake of fiber, depression, visceral fat, and a BMI greater than 30.
It’s important to note that other conditions linked to GERD increase at midlife. For instance, people with sleep apnea frequently have GERD and GERD is a risk factor for sleep apnea. And treating sleep apnea improves GERD.
Untreated thyroid dysfunction can also cause digestive issues through esophageal motility disorders, such as GERD. Hyperthyroidism can decrease acid production. Luckily, symptoms resolve with treatment.
Breathing disorders such as COPD and asthma also up the risk. Poor breathing in COPD can compromise the crural diaphragm, which negatively affects the anti-reflux barrier.
Autonomic dysfunction, particularly reduced parasympathetic tone, is strongly associated with GERD. In one small study with 29 GERD patients, 44.4% had severe autonomic dysfunction and 79% had impaired parasympathetic functioning, compared to controls.
Between 10-33% of people with GERD also have decreased gastric emptying. Here, the anti-reflux barrier opens because food is staying in the stomach longer than it should.
So, let’s examine what can go wrong with gastric motility.
Reduced gastric motility
The GI tract and the brain communicate with each other, which is referred to as the Brain-Gut axis. This happens via the enteric nervous system, which are nerves that line the stomach, primarily through the vagus nerve.
The vagus nerve contains 75% of the parasympathetic nervous system nerve fibers. That's why we say the parasympathetic nervous system helps bodies rest and digest. They innervate the stomach and have special “nitrergic” neurons that handle gastric motility.
First is gastric accommodation, which is a reflex that allows food to be stored temporarily by relaxing smooth muscle. This is followed by peristalsis, which involves electrical slow waves.
This process of peristalsis depends upon nitric oxide, which is produced by nitrergic neurons. Back to the heart analogy. I’ve talked a lot about the endothelial nitric oxide synthesis (Enos) which makes nitric oxide in endothelial cells that line blood vessels to enhance blood flow.
Well, in nerve cells, the enzyme neuronal nitric oxide synthesis (Nnos) makes and releases NO to regulate gastric motility. Researchers know this because when they give animals drugs to block Nnos, their stomachs become grossly enlarged.
Emerging research suggests sex hormones also influence gastric motility. Although estrogen increases Enos to enhance blood flow, it is believed that the opposite occurs in the GI system. Estrogen decreases Nnos, resulting in a delay of gastric emptying.
In fact, researchers believe that estrogen relaxes the anti-reflux barrier, which could explain why pregnant women and those on hormone therapy tend to experience more GERD.
A benefit of estrogen, though, is it protects the esophagus from damage when or if GERD occurs, leading to a lower risk of esophageal cancer.
This may be why gastroparesis–delayed gastric emptying- is more common in women than men (4:1). Symptoms of gastroparesis include nausea, vomiting, early satiety, bloating and abdominal pain. It’s also more common in type 2 diabetes, which can damage nerve cells in the stomach.
The same way stress makes our heart beat faster, it also affects the stomach and intestines. We’ve all felt physically ill with short-term stress, which can cause stomach pains and loose bowels.
Although food will stay longer in the stomach because of the increase in fight or flight sympathetic tone, colonic motility increases, which is why we simultaneously find ourselves in the bathroom more.
Aging pause and its subsequent increase in sympathetic activity play yet another role in motility issues. As blood flows elsewhere during flight or flight, food simply stays longer in the stomach.
We've discussed the relationship between the anti-reflux barrier and stomach motility. But what about the stomach’s mucus layer and HCL? How do they shape up as we age?
Changes go the gastric mucosa (and HCL)
After the age of 60, one out of three people have atrophic gastritis, a condition that leads to inflammation and thinning of the stomach lining. One out of three!!
Why does this happen? It’s multifactorial, but there are two leading factors. One is because of an autoimmune reaction, where antibodies attack the stomach lining. And the second, and more common, is the result of a Heliobacter pylori (H pylori) infection found in 50% of adults worldwide.
Researchers used to think declining stomach acid and function was an inevitable part of aging, but the discovery of H. Pylori changed that.
H pylori is bacteria that grows in the stomach. It can damage the stomach lining, causing inflammation in both the stomach and in the duodenum, the first part of the small intestine.
In fact, by the time we reach 70, most of us (60%) will have H pylori even though many will be asymptomatic. H pylori is a risk factor not only for atrophic gastritis but gastric cancer and peptic ulcer disease. According to Kaiser Permanente division of research, H. pylori is responsible for ninety percent of gastric cancers.
H pylori produces the enzyme urease, which neutralizes stomach acid. Hypochlorhydria is when the pH of the stomach is >4 and achlorhydria (no stomach acid) occurs when the Ph is >7. As many as 30-40%, of postmenopausal women have compromised stomach acid production.
Inadequate HCL increases the risk of small intestinal overgrowth (SIBO) which is when a high number of bacteria live in the small intestine. That’s because the stomach can’t do its job of killing pathogenic bacteria, but it also can’t completely break down food, including protein, which can cause bloating and indigestion.
Researchers don’t know exactly what causes H Pylori to increase with age. This is an area that requires much more research. I wonder if a lower amount of nitric oxide in the stomach - and overall— is a contributing factor. Acidified nitrite, which turns into NO, is antibacterial and at certain levels kills H pylori.
I found one study that included 638 patients with chronic atrophic gastritis who were admitted to the hospital. Those with h pylori (80%) were more likely to be older, have a family history of gastric cancer, have muscle wasting, or be at a higher weight, drink alcohol, consume strong tea, have more work pressure, a high intake of fish and a low intake of dairy, fruits, and vegetables.
Since this is only one study and it's with hospitalized patients, it may not apply to everyone.
You can think of H pylori like plaque buildup in arteries which, by the way, can survive in a low Ph. Environment of the stomach. Yet unlike heart disease, the medications prescribed–or over the counter — can make things worse.
The medication trap
When stomach issues such as GERD come up, doctors are most likely to prescribe proton-pump inhibitors (PPIs). You can also find PPIs over the counter.
PPIs block the production of HCL in the stomach, keeping the pH. around 4-6. This can help with healing ulcers and preventing progression/complications of GERD, such as Barrett’s esophagitis. Yet when taken long-term, it leaves the stomach in a hypo-functioning state.
Despite being meant for a short duration (up to 12 weeks or as prescribed), PPIs are frequently used long-term (>1 year). In fact, they are one of the most frequently prescribed drugs (100 million annually).
One study found that 25 to 75% of patients taking PPIs don’t have an appropriate indication. Doctors often discharge hospitalized patients on PPIs without a plan to stop them.
Long-term use >3 years has been shown to increase the risk of atrophic gastritis, micronutrient deficiencies (especially B12, magnesium and calcium), high blood pressure, dementia, chronic kidney disease, community acquired pneumonia, and C diff associated disease (CDAD).
In a study with 80,000 postmenopausal women, those taking PPIs greater than two years had a 35% higher incidence of hip fracture and 42% and 52% in those take it for 4 and 6 years. The good news is that the risk decreases once they stop taking it.
Researchers point to decreased absorption of calcium and magnesium as potential reasons for increased fracture risk. But it could also be because of decreased NO, which also plays an important role in bone health.
Another medication that affects the stomach is non-steroidal anti-inflammatory agents (NSAIDS) which people take more of as they age. NSAIDS inhibit the production of prostaglandins which help protect the stomach lining and increase the risk of ulcers.
Don’t get me wrong. These medications can be necessary, but we need to be careful because they are being prescribed frequently, without proper follow up.
What midlife women can do
Much of the fine-tuned healthy lifestyle advice I talk about can help reduce the risk of stomach issues and may even help when symptoms begin, but let’s get into specifics.
First are vegetables rich in nitrate to help increase NO in the stomach, which increases blood flow and thickens the mucus layer. The two-a-day nitrate veggie challenge can be helpful in protecting the stomach.
Adequate fiber is linked to a decreased risk of GERD and increased motility, as well as better health. See this post for how to meet your fiber needs. And probiotics also help decrease the risk of h pylori so don’t miss my post on fermented foods.
Ensuring micronutrients may be helpful, but the evidence is sparse. In particular, zinc seems to have a protective effect on the stomach and plays a role in HCL secretion. See this post about zinc.
Sleep and GERD have a bi-directional relationship. Getting over 7 hours of sleep is helpful as is avoiding eating three hours before bed.
Although evidence is mixed on the impact of food types (spicy, coffee, etc.) and lifestyle on stomach issues such as GERD, individuals should avoid consuming large meals or eating past fullness, consuming very high fat meals, consuming high amounts of salt, and consuming excess alcohol.
Working on stress reduction is key. So is slow, and deep breathing to stimulate the vagus nerve, allowing for adequate NO and gastric motility.
There is evidence for slow, diaphragmatic breathing for reducing symptoms of GERD and inspiratory muscle strength training (IMST). The latter helps strengthen the diaphragm, thus improving the anti-reflux barrier.
When problems persist, the key is to find a health professional who will help you get to the root of the problem.
Medications may be needed for healing or while tests are being done. H. Pylori eradication therapy may be part of that. Be sure to ask questions so you can understand where the problem is coming from.
If you are put on PPIs (or H2 blockers) ask how long you should be on them and what tests you should get.
Ask about your risk of other health conditions that could make the problem worse, like sleep apnea, thyroid dysfunction, autonomic dysfunction, and diabetes. Now might be a good time to get a dexa to check bone density.
And if you have micronutrient deficiencies with no explanation, ask about a referral to a GI specialist to check for stomach issues like H Pylori. We know that low stomach acid can result in iron, magnesium, vitamin B12, vitamin C, calcium, and vitamin D deficiencies.
If it is determined you have low stomach acid or autoimmune atrophic gastritis, ask your healthcare provider if you’re a candidate for taking Betaine hydrochloride to replace acid, which can work well for some people.
This isn’t meant to replace medical advice, but to arm you with information to help you when you seek help.
So many questions left unanswered
This was a doozy to write. And even though it’s not something I can tie in a bow and say just do this, I wanted to put it out there.
As for me, I rarely get those stomachaches these days. This may be because of my efforts to decrease stress and anxiety levels. Or that my hormones no longer fluctuate wildly. Maybe it’s my breathing routine or how I work to increase NO in my diet. Who knows?
The secret may be in all the little things we do. Either way, it helps to be informed if we seek help from a medical provider. We need to speak up if they just offer medication with no digging.
The same is also true if a functional doctor recommends a bunch of supplements or some type of protocol. Understanding why and the science behind it is important.
Try to determine which part of the Fab 4 is compromised and what is causing it. Let’s hope we learn more about stomach health the same way we've learned about heart health.
Have you experienced stomach issues in midlife? Let's talk about stomach issues in the comments!