
Happy late Mother’s Day! It has been a crazy May already, and it’s just getting started.
As usual, I’m keeping tabs on articles and studies for midlife women. Here’s what I got for you!
Disappointing news on vitamin D
A couple of articles in JAMA touch on vitamin D, including a summary of the Endocrine Society’s most recent recommendations.
Then I remembered I wanted to write about these recommendations.
The panel examined randomized placebo control trials on what they call empiric vitamin D supplementation, which is an amount which exceeds the RDA of 800IU.
They conclude that empiric supplementation is beneficial in children 1-18, people over 75 and during pregnancy. They say there is no clear evidence for a target blood level of vitamin D or screening for vitamin D deficiency.
Apparently, vitamin D stops being beneficial between 19-74. They can’t even pinpoint an optimal dose for people as they write:
Because the vitamin D doses in the included clinical trials varied considerably and many trial participants were allowed to continue their own vitamin D-containing supplements, the optimal doses for empiric vitamin D supplementation remain unclear for the populations considered
So, we still don’t have answers. According to the 2021 recommendations from the United States Preventative Task Force, they don’t recommend screening because “No studies directly evaluated the health benefits or harms of screening.”
There are no recommendations for the type of research to get answers, just insufficient evidence. This is so sad, and I’ll tell you why.
We don’t hold this same standard with other screening tests
Doctors routinely check liver enzymes, kidney biomarkers, and red blood cell counts—even though there’s little evidence that these tests prevent chronic disease. So why do we do them? It’s common sense: we want to know how the body’s major systems are working.
But for screening micronutrient levels, like vitamin D, we don’t apply the same logic.
This is true even though we know many of us are at risk of vitamin D deficiency. Food alone doesn’t provide enough—98% of people fall short without sunlight or supplements. Historically, low vitamin D led to rickets in children, a condition once common and life threatening but now preventable.
Vitamin D isn’t just about bones. Nearly every cell in the body has a receptor for it, and it plays a role in immune function, brain health, and controlling inflammation.
Despite this, routine screening for vitamin D is not recommended. Meanwhile, doctors perform liver function tests on everyone, even though only 1–4% of asymptomatic people show elevated enzyme levels.
Compare that to vitamin D. Recent NHANES data shows that 25% of Americans have levels below 20 ng/mL. Women, people in winter months, non-Hispanic Blacks, and adults aged 20–29 are at the highest risk.
Most health experts agree that levels below 20 ng/mL (<50 nmol/L) are problematic, and linked to poor bone health, fractures, and bone loss. Severe deficiency (below 12 ng/mL/25 nmol/L) is even more serious, increasing the risk of death, infections, and other diseases.
So, what do we do? We keep checking those liver function tests and don’t recommend screening for vitamin D, even though 1 out of 4 are deficient (eye roll).
Bear with me, as I make one more point.
READ: The importance of vitamin D during the menopause transition
Researchers poorly design micronutrient/supplement studies
Randomized control trials work great for drugs. In these trials, participants receive a drug—something not already present in the body—or a placebo, which is an inactive substance. Researchers then measure biological markers, like LDL cholesterol in the case of statins, as well as health outcomes such as heart attacks or strokes.
This model is often used for micronutrient supplements, but it has limitations. Unlike drugs, micronutrients like vitamin D are already present in the body and are essential for health. This complicates the study design.
They also bend the rules by not testing micronutrient levels at the start and end of the study. Many vitamin D studies give vitamin D supplements to those replete in vitamin D. This would be like studying a blood pressure medication on people with normal blood pressure.
Ethically, they can’t deprive one group of that micronutrient, so they usually allow them to take at least the RDA. Also, they can’t control for sun exposure, which is a major source of vitamin D.
And last, everyone’s response to vitamin D supplements differently. One can get there levels up with 2000 IU and another might need double or triple that.
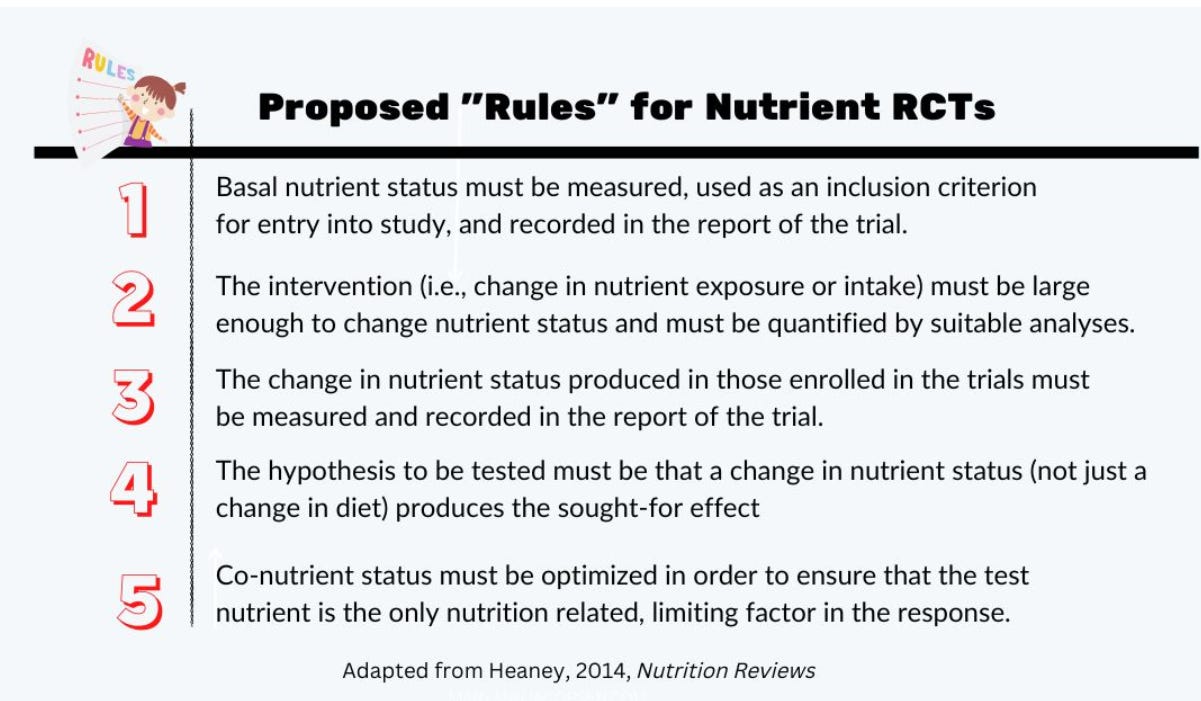
These issues have prompted researchers to promote careful design in nutrition studies. In 2014, Robert Heaney presented guidelines for nutrition studies shown below.
“The change in nutrient status produced in those enrolled in the trials must be measured and recorded in the report of the trial,” he wrote. “The hypothesis to be tested must be that a change in nutrient status (not just a change in diet) produces the sought-for effect.”
This idea of nutrient measurement that Robert Heaney emphasized over 10 years ago is something many health professionals and researchers believe is the missing key in the vitamin D clinical research literature.
If we designed research this way, perhaps we could determine the ideal level we need, just like we know the ideal levels for liver enzymes.
Okay, I feel better now.
Is breathing going mainstream? (and other cool articles)
I ran across these two articles on breathing! The first article focused on midlife women: Breathwork is the hormone-friendly anti-ageing practice going mainstream.
The article isn’t very deep, but it mentions breathwork is becoming a popular tool for women.
There was also a NY Times article: The Science is Clear: Deep breathing can be a game changer for anyone. Elite athletes agree.
This piece goes in depth and focuses on how many athletes use deep breathing to enhance their sport. I like how it highlights the science and how clear it is…. hopefully this is catching on:
“To some, it may seem puzzling. It’s just breathing, right? The science, however, is quite clear, according to Nicholas Tiller, a researcher at the Lundquist Institute at Harbor-UCLA Medical Center. Using a regular deep breathing routine can reduce your anxiety, blood pressure and heart rate while improving your overall mental health.”
- Rustin Dodd, May 1, NY Times
Learn how to cultivate your own breathing practice!
Another NY Times article, “17 Ways to Cut Your Risk of Stroke, Dementia and Depression All at Once,” highlights data from 59 meta-analyses.
First it focuses on factors that lower the risk of brain diseases including low-to-moderate alcohol intake, cognitive activity (reading/puzzles), a diet high in fruits, vegetables, dairy, fish and nuts, physical activity, a sense of purpose and a large social network. Read the rest to see what increases risk (no big surprises).
There are a couple of articles you need to check out on Substack.
First, a must-read post from Ann Marie at Hotflash Inc., Why I’m not buying into the cult of all or nothing anymore. I think the title says it all. And Jen Gunter explains the importance of iron deficiency in perimenopause. A doctor who gets it…nice!
May means letting go
My oldest graduates high school in less than two weeks, which is why my posts have been erratic.
I’ll leave you with two articles. One is an essay from Anna Quindlen I read every Mother’s Day, On Being Mom. And the other is from Tiny Buddha about How to make the most of our time with people we love (thanks Ris).
Have a great rest of the month!





Congrats on the graduation! Enjoy and bring tissues!