Women’s health research initiative, CBT for hot flashes, and the golden bachelor
December midlife roundup
The beginning of December always freaks me out. The amount of stuff to do is overwhelming, but it always gets done. This year I want to focus on really enjoying the holiday season and not get bogged down with the to-dos.
Deal? Deal.
Now to updates…
The White House and Women’s Health
On the same exact day I posted about the gaping hole in women’s research, the White House announced its women’s health research initiative. Say what? This is being led by first lady Jill Biden.
According to the White House website, the mission of the initiative is as follows:
Despite making up more than half the population, women have historically been understudied and underrepresented in health research. The new Initiative will fundamentally change how we approach and fund women’s health research, and pioneer the next generation of discoveries in women’s health.The Initiative is committed to galvanizing the Federal government and the private and philanthropic sectors to spur innovation, unleash transformative investment to close research gaps, and improve women’s health.
Initiative members are making recommendations to the Biden-Harris administration within 45 days. They are also taking comments and recs from the public, so I’ve been spending time on a piece to submit that I also hope to get published, which is why I didn’t send a newsletter last Monday.
This is all great news and I hope women's health gets the attention it deserves. And I especially want midlife health to be a focus.
New Nice and CBT Guidelines
The UK’s National Institute for Health and Care Excellence (NICE) updated their treatment recommendations for menopause symptoms. They now recommend cognitive behavioral therapy (CBT) along with HRT or alone. Research shows it can help with mood, hot flashes, and sleep.
“This update includes important evidence-based information to help both women and healthcare practitioners during their discussions about the best treatment to manage their symptoms,” said Professor Gillian Baird, the menopause guideline committee chair in a press release. “This gives women more choice and enables them to make informed decisions for their personal circumstances.”
I’ve talked about CBT before and have personally used it to help with anxiety. CBT focuses on our reaction to an event, including our thoughts and how we cope. For example, if we start having symptoms of a panic attack and we tell ourselves we might die, this makes the anxiety rev up considerably. Then, as a coping skill, we might avoid the things that make us anxious, which only makes our anxiety grow.
In terms of menopausal symptoms, we can also change our reaction and how we cope. This helpful pdf handout on CBT from the British Menopause Society provides examples:
Women with the highest levels of distress in reaction to hot flushes tend to ‘catastrophise’ about the hot flush, i.e. think the worst. They are more self-critical within the situation, especially about their appearance.
There has been a negative reaction to these new guidelines. Some menopause experts and influencers believe this is a setback in menopausal health, and may cause doctors to deny women the hormones they need.
But how can evidence-based recommendations ever be wrong? Should we withhold information because not everyone agrees with them?
Talk about a setback!
No one seems to be talking about why CBT is helpful. Of course, I have my theory. This is not about symptoms being in our head. In fact, women who experience more intense menopausal symptoms are at higher risk of cardiovascular disease compared with those who don’t.
Even in a day and age where we talk a lot more about the impact of emotional health, we’re still missing the boat. Some studies show that CBT can reduce levels oxidative stress and inflammation (these two things go together). Research also links menopausal symptoms to oxidative stress. So perhaps in this way, CBT helps decrease the negative effects of hot flashes.
In short, sex hormones (thankfully) are not the only influence on our physical health as midlife women, our emotional health matters too. It doesn’t have to be an “either/or” situation, as women can benefit from both. CBT teaches us how to better cope with these changes and women need to know this! Period.
New Keeps Update
I recently posted an update to the Keeps trial on Instagram, which is the first randomized trial to compare oral estrogen to transdermal estradiol with both women taking progesterone. The hormone group continued the treatment for four years, and researchers followed all the subjects for 14 years.
This population was in good cardiometabolic health at the onset and started MHT within three years of menopause. Average age was 54 at the start and 67 after 14 years.
This recently published finding found no significant difference in the two groups after 14 years in various measurements (blood pressure, HOMA-IR, HDL, glucose, triglyceride etc.) The only difference was women in the placebo had a higher rate of diabetes. But this did not show up in lab measurement differences. They were also similar in adverse events such as stroke, fracture, cancer, etc.
The researchers conclude:
There was no evidence of long-term cardiovascular or metabolic benefits, nor any evidence to suggest adverse effects associated with remote exposure to HT initiated proximate to onset of menopause and administered over a 4-year period in overall healthy postmenopausal women with good cardiovascular health.
Is this the last word on estrogen and cardiovascular health? No. I doubt we’ll ever get concrete answers because this is hard to study and so many other factors go into heart health. But overall, it found a neutral effect.
What this tells me is that, so far, hormones are also not the answer to the metabolic health issues of midlife women. Whether women take hormones, we all benefit from making strides to improve our health and wellbeing.
PPIs in the news
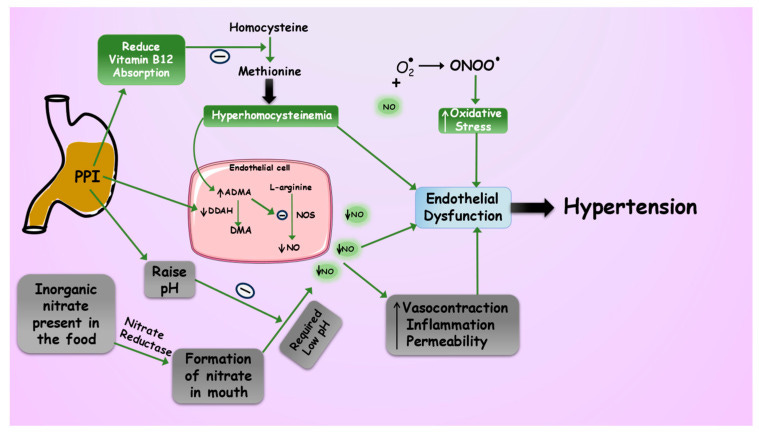
I also posted a reel on Instagram about the potential harms of using proton pump inhibitors. A recent review in Pharmaceuticals hits on the potential reasons proton pump inhibitors can increase the risk of cardiovascular disease, especially hypertension.
These medications work by limiting the amount of acid that proton pumps in the stomach induce. Yet we need stomach acid for a variety of functions. In the study, researchers discuss how PPIs increase a substance called AMDA which increases endothelial dysfunction, the precursor to heart disease.
They decrease absorption of vitamin B12, iron, magnesium, and zinc. Low B12 and zinc can lead to elevations in homocysteine. Because we need stomach acid to make nitric oxide (NO) from nitrates in foods like leafy greens, we have less production of this magic molecule.
Taking PPIs for more than 4 years was associated with a 30% higher risk of Alzheimer's disease, according to a 2023 study in Neurology. Not only that, but a 2022 systematic review and meta-analysis reveal that all studies showed an increased risk of fractures in menopausal women who took PPIs for 12 or more months.
There are no studies on PPIs and menopausal symptoms, but my guess is there’s a link. Now, you can buy PPIs over the counter without needing a prescription, such as Prilosec and Omeprazole!
These meds were never meant to be lifelong medications. For instance, taking them to help the stomach heal from an ulcer or decrease GERD symptoms while searching for the cause. But now long-term use of these meds causes obvious harm.
If you’re on a PPI, be sure to talk to your healthcare provider about the potential risks.
The Golden Bachelor AHA
I didn’t watch all the Golden Bachelor but recently caught up on the highlights on YouTube. I started it with my teen daughter, but she lost interest.
As I was watching it recently, I had this aha. I wondered why they chose a bachelor in his early 70s and all the women were 64 plus years old. They could have chosen a midlife bachelor, right? Maybe it wouldn’t be golden, although the golden girls were of midlife age.
But I think this show mirrors society (and research) on adults. The regular show has people in their 20s and 30s. Golden bachelor has people 64 plus. But what about those in the middle 40-65—left out of the equation once again? Not young or old enough.
What do you think? Would you like to see a midlife bachelor or bachelorette?? (and research too, ha ha)
Links
I’ll leave you with a few articles that caught my eye:
Clarissa Kristjansson from the Heart of Menopause shares how she left her corporate job to start her own business in Milestones, Memories and Menopause
Over at Nutraingredients: Menopause: Women’s health at risk due to avoidable nutrient deficiencies (YES!!)
Carla Digirolamo from Athletic Aging sums another study on hormone therapy Hormones for the Long Haul - the Jury is Still Out.
Last is an article in the NYT about weight loss drugs. I plan to post about this! A New Match for Menopausal Weight Gain: Ozempic





