Is your blood pressure rising in midlife? Here’s what to do
A complete guide to understanding and addressing rising blood pressure
Short on time? I’ve added a HIGHLIGHTS section at the end with the key points.
“I really need to lose some weight,” said the middle-aged nurse, speaking about her blood pressure inching up.
“Do you think that’s the reason?” I asked.
“Of course,” she said, like I should know better being a dietitian. But she was a petite woman and even though that was years ago, I think her response gets at how society views blood pressure….just lose weight!
When I had my blood pressure scare, I set out to learn everything about blood pressure. Now, I see blood pressure differently than I did before.
Midlife women of all sizes are prone to high blood pressure with age. From ages 18 to 39, only 13% of women have high blood pressure. This jumps to 50% at 40-59 years of age and over 60 its 73.9%.
Since high blood pressure impacts many of us, let’s dive into the details in part 1 of this two-part series on blood pressure.
Blood pressure 101
As the heart pumps blood, arteries widen or narrow to meet the body’s demand. Blood pressure is the force that blood exerts on artery wall.
Different systems are at play in maintaining a healthy blood pressure. You have the renin-angiotensin-aldosterone system (RAAS) producing compounds like angiotensin II and aldosterone, which constrict blood vessels, increasing blood pressure.
The vasodilator system comprises endothelial cells that line blood vessels. They release nitric oxide (NO), which relaxes and widens blood vessels, resulting in decreased blood pressure.
Also on the job is the baroreflex, which has specialized neurons called baroreceptors that work to normalize fluctuations in blood pressure through the autonomic nervous system.
For instance, when you’ve been sitting and your blood pressure is low and you suddenly stand up, baroreceptors message the brain, which causes a jump in heart rate and vascular resistance.
For most of our younger years, these systems work seamlessly and blood pressure at rest is <120/80.
But with aging pause, many women experience elevations in vasoconstriction, decreases in vasodilation, and reduced baroreflex sensitivity. This raises blood pressure at rest and the health risk that goes along with it.
Get a true reading at home
Step 1 is understanding your blood pressure at rest. Blood pressure at the doctor’s office tells you your BP in the office, but not real life.
Taking your blood pressure at home is more reliable according to the 2019 American Heart Association (AHA) position stand, “Several studies have shown that BP on home blood pressure measurement (HBPM) maintains a stronger association with CVD risk than office BP.”
HBPM can also help you understand if you have white-coat hypertension, blood pressure phobia (like me), or even masked hypertension, which is a normal BP at the doctor’s, but high in real life (10% of people have it!).
If you get nervous at home, buy a monitor which takes three in a row and averages and stores them. Don’t look at the number and take it multiple times so you can really relax.
Even the act of taking blood pressure at home has a positive impact on BP. But most importantly, it will give you a good idea of your blood pressure in real life.
Understand why midlife is a vulnerable time
Since the 1940s researchers have noted BP differences between men and women. Yet the mechanisms have only recently come to light.
Estrogen has a vasodilator effect as it stimulates NO release while testosterone stimulates the RAAS system, which is why premenopausal women have lower BP.
Fluctuations in the components of the RAAS occur during the menstrual cycle and are influenced by estrogen.
Compared to age-matched men, women are also more vulnerable to reduced baroreflex sensitivity (BRS) with aging. Women experience increases in sympathetic activity after 30, jumping even higher after 50.
Hello anxiety!
Researchers examined BRS of 105 premenopausal and early postmenopausal women ages 40-55. Early postmenopausal women exhibited increased sympathetic activity and decreased BRS.
Not only that, but this lower BRS response predicted prehypertension.
Menopause plays a role
It’s easy to blame declining sex hormones on rising BP, but remember that One Health Principle. Many factors, including aging and sex hormones, can affect the decrease of nitric oxide, which increases inflammation and oxidative stress and vice versa.
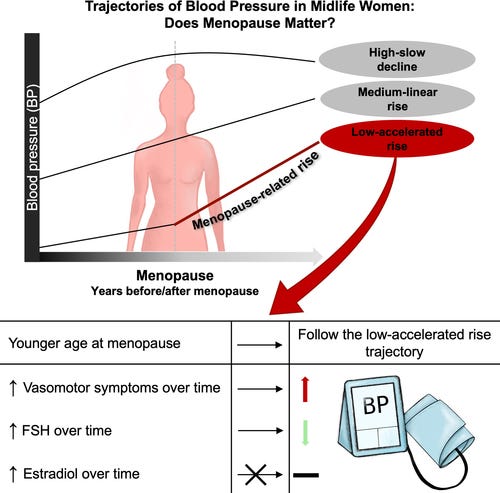
The SWAN study attempted to answer the how-does-menopause-affect-BP question by following 3302 multi-ethnic women’s blood pressure over 17 years.
The researchers classified blood pressure results into low-accelerated, medium-linear rise, and high-slow decline trajectory groups. Thirty-five percent of women were in the low-accelerated rise one year after the last period, showing an increase because of menopause.
Most women, (about half) in the medium group, showed a linear increase over time and no rise at menopause. And the last group, which had higher blood pressures, actually saw a slight decline after menopause.
Researchers did not find any influence of estradiol levels on blood pressure, but they did for younger age at menopause, FSH and menopause symptoms.
Studies with hormone therapy are also mixed, showing estrogen lowers BP in some women and increases it in others. The Replenish RCT with estradiol and progesterone showed a neutral effect on BP.
Women are at higher BP risk than men
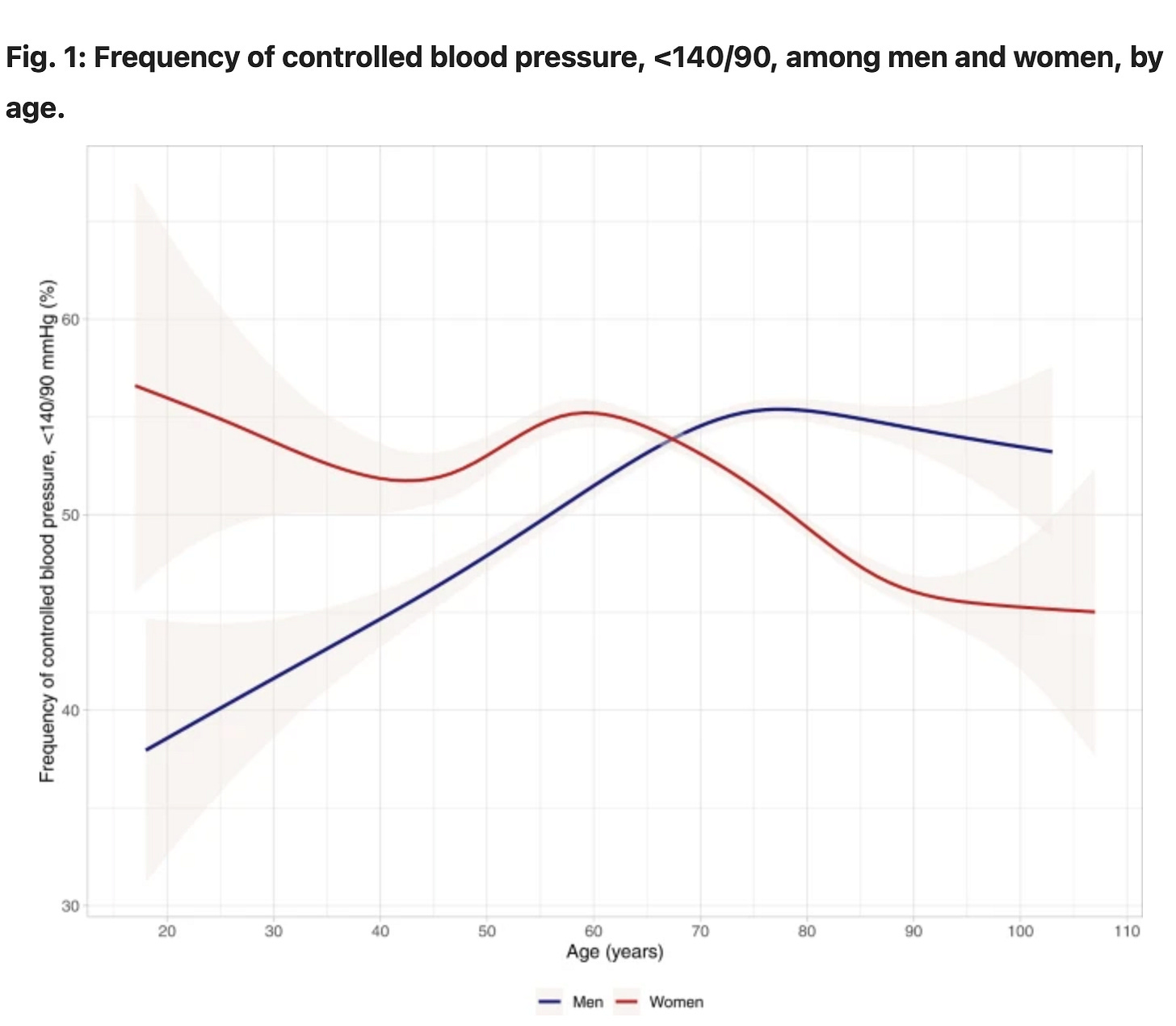
Women have lower blood pressure than men until after 60.
For instance, while only 13% of women 18-39 have high blood pressure, 31.2% of men do. This goes up substantially to 50% at 40-59, almost catching up to 60% of men. But after 60, it’s about equal (75.2 vs. 73.9%).
When women’s blood pressure rises, evidence suggests they are at higher cardiovascular risk than men.
In a study in the journal Hypertension last year with 53,000 people, women were at higher risk of cardiovascular deaths with a systolic blood pressure 12 points lower than men.
So, we midlife women need to stay on top of blood pressure, as it presents a unique set of risks.
The consequences of elevated blood pressure between males and female again appears sex-specific, and there is emerging evidence that hypertension is a more potent cardiovascular risk factor in females. - Connelly et al, 2022, Hypertension and the Kidney
Advocate for yourself to find the WHY
As Jenn went through menopause, her blood pressure increased at the doctor’s. She was told most women at menopause need medication. Her mother also had high blood pressure.
Brewing underneath were changes to her thyroid as her TSH was rising and her cholesterol and triglycerides. This decreases nitric oxide release and increases oxidative stress, disrupting The One Health Principle.
Stacy lost weight and was happy to get off her blood pressure medications. Yet later, when Stacy was no longer actively losing weight, she felt awful with tingling in one arm and went to the ER. They found her blood pressure to be 180/100 and put her back on her medications.
Doctors did not discover her undiagnosed sleep apnea until 10 years later. With sleep apnea, low oxygen levels increase oxidative stress/inflammation and decrease nitric oxide. In fact, 50% of people with high blood pressure have sleep apnea and vice versa.
It’s always a good idea to check these underlying conditions—especially sleep disordered breathing — which could contribute to high blood pressure. Here are some to consider:
Sleep apnea, snoring, and upper respiratory resistance syndrome all are linked with elevated blood pressure. Ask your doctor to get tested and be sure you test oxygen levels during sleep.
Both high uric acid and homocysteine are linked with increased blood pressure, they are also elevated in people with sleep apnea.
Check thyroid function, looking for trends from previous years
Ask the doctor to check for primary aldosteronism, which occurs when the body secretes an excessive amount of the vasoconstrictor aldosterone, leading to secondary hypertension. About 5-12% of people with hypertension have this.
Understand the limits of medication
Some women will need medication to help keep their BP under control. Yet only about half of people who take medication have well-controlled blood pressure. And by that, I mean they have blood pressures <140/80, which is too high for women.
Women show better control of blood pressure until after age 60, where it’s reversed and men have better control, as shown below.
The result of the Sprint study found benefits to tight control (<120/80) in patients with high blood pressure. However, most people are not achieving that goal, and I believe it is a mistake to depend solely on medication to lower blood pressure.
There are different medications for blood pressure. Diuretics help decrease salt and water retention to lower blood pressure. Calcium channel blockers prevent calcium from entering the heart and blood vessels, helping vessels dilate.
ACE inhibitors block vasoconstricting pathways and beta blockers slow and decrease the force of the heart. These medications can reduce the risk linked to high blood pressure and enhance endothelial function.
But, and this is a big but, most medications don’t get at a key aspect of blood pressure in women: the loss of the vasodilator nitric oxide.
A 2021 review summarizes the lack of success in finding BP drugs called NO donors, with new ones expected soon.
The balance between the levels of NO and Ang-II seems to be a central aspect in CVD, especially in the pathogenesis of hypertension…Based on the important properties of NO, NO donors were produced and have been used for the treatment of vascular disorders. However, due to the side effects presented by these donors, particularly vascular tolerance, new molecules have emerged with the potential to be used in the treatment of cardiovascular diseases.
NO donors like nitroglycerin work great initially, but people develop a tolerance and can even worsen vascular health.
Watching weight and sodium is not enough
Let’s revisit the nurse who believed that the 5 pounds she gained were raising her blood pressure.
Short-term weight loss reduces blood pressure, but it’s most likely because of the decrease in calories which reduce insulin. A reduction in insulin decreases BP. For example, many bariatric patients’ blood pressure decreases a week after surgery, well before they lose weight.
There’s a lack of studies on the long-term effects of weight loss. A 2021 study with 278 people, average age 48, measured BP at 6 months and 18 months during and after a weight loss intervention. BP decreased at 6 months but at 18 months went back to baseline, even with no change it weight.
It’s true that visceral fat is linked to high blood pressure because it increases inflammatory markers and weight loss can help lower it. But exercise does a better job.
Reducing sodium can also lower blood pressure. But underneath the jump in salt sensitivity at midlife is the reduced ability for blood vessels to dilate and increase NO with high sodium intake.
Even in normotensive individuals, seven days of a high salt diet dampened vascular responses, so we all need to watch sodium. But reducing salt doesn’t get to the key issue.
From understanding to action
The goal of this post is to help you understand the why behind blood pressure, get an accurate reading, and rule out conditions associated with BP.
Highlights:
· Half of midlife women 40-59 will see a rise in blood pressure beyond 130/80.
· Taking blood pressure at home is more reliable than BP taken at the doctor’s office.
· Blood pressure is an imbalance in blood vessel’s ability to dilate (nitric oxide-NO) and constrict (angiotensin II).
· Aging, increases in sympathetic tone, lifestyle, and declining sex hormones (decreased NO), play a role in rising blood pressure in midlife women. Yet menopausal hormone therapy has a mixed or neutral effect on BP.
· Health conditions that also increase at midlife such as sleep apnea, thyroid dysfunction, and increased biomarkers (homocysteine and uric acid) also play a role, so check with your healthcare provider.
· Primary aldosteronism is a less common cause of high BP but is underdiagnosed and should be ruled out as a cause of secondary hypertension.
· Medications can help lower blood pressure, but don’t directly increase vasodilation (NO), the major issue in women; that may change as new drugs become available.
· Weight loss and reduced sodium can help but will not solve underlying issues tied to rising blood pressure.
Send this post to a friend who may not understand why her BP is rising. Stay tuned for part-2 post, where I’ll cover different approaches to lowering blood pressure and the expected systolic reduction from each.
Let’s talk about your experiences with blood pressure in the comments!





I had a sudden increase in blood pressure at 45. I find the act of taking my blood pressure stressful, even at home.