
This information is meant for education and not a substitute for medical advice.
When I first started researching midlife, I was hoping to get concrete answers about whether to take hormone therapy.
Now I’m at the point where I’ve gone 6 months without a period and I’m still not sure.
So I thought I’d rehash some key points I’ve learned along the way, debunk some claims, and reveal the results of an intriguing new study.
The no brainers
At the start of my research journey, a few things became evident. First was that the now infamous Women’s Health Initiative study done in the early 2000s had some major holes.
The average age of the participants was 63 and most of the increased risk to heart disease and cancer was in women over 60 or greater than 10 years from menopause.
This is known as the "timing hypothesis," which shows that taking hormone therapy closer to the time of menopause and at younger ages reduces this risk.
Organizations like the Menopause Society, Endocrine Society, and the American College of Obstetricians and Gynecologists support the use of hormonal therapy in symptomatic midlife women, stating that in younger women without contraindications (10 years from menopause) the benefits outweigh the risks.
Also, the research reveals that vaginal estrogen does not carry the same risks as menopausal hormone therapy (MHT) because it remains local, resulting in minimal absorption. I didn't waste any time when I experienced vaginal symptoms after three months without periods, and I began using it.
Last is that women who go through premature (<40) or early (40-45) menopause, including surgical removal of the ovaries, are at increased risk of multiple health conditions. Unless contraindicated, hormone therapy is recommended until at least until the natural age of menopause (around 51/52).
These were no brainers. But there was another point that wasn’t so clear I want to touch on.
Progestogens are the general category that includes synthetic progestins and progesterone commonly given with estrogen in women with a uterus (EPT), women without a uterus are given estrogen alone (ET)
What if you don’t have symptoms (or they are minimal)?
Since I haven't had a period in 6 months, I've been experiencing mild symptoms, mainly feeling clammy upon waking up. I have experienced “warm flashes” but it's not continuous. Basically, it’s just feeling warmer than usual upon waking.
But other than that, I’m still sleeping well and feel pretty good. So the question is, will taking hormones improve my health or prevent future issues? This is a subject that comes up a lot on social media.
The claims that hormone therapy decreases the risk of heart disease, dementia, osteoporosis and helps women live longer are everywhere. But not only that, some say menopause is a “default” state of inflammation.
Before we check the research; I want to say I get the significance of this story. I mean, we mature as young girls with the help of sex hormones, especially estrogen. When they eventually fluctuate and decline, it’s also a time health issues rise. Why wouldn’t we look to estrogen?
In 1966, in the book Feminine Forever, Doctor Robert Wilson argued that estrogen is the natural way to maintain femininity, health and well-being. He flew around the country promoting it and prescriptions for hormone therapy skyrocketed. Later, investigators discovered that the pharmaceutical industry funded all his expenses and research foundation.
Estrogen received its first bad hit when reports started circulating that it caused endometrial cancer. And by April 1978, every estrogen package required a warning label. Soon evidence revealed that adding a progestin (synthetic progesterone) prevented estrogen-induced endometrial changes.
Use of estrogen — and progestin — increased in the 80s and 90s. Along the way, it was found that estrogen helped prevent osteoporosis in addition to treating menopausal symptoms like hot flashes.
During this time, it was also believed that hormone therapy reduced the risk of heart disease. After a landmark meta-analysis in 1992, the American College of Physicians published a position stand statement recommending that all postmenopausal women be offered hormone therapy to help prevent heart disease.
Then the Women’s Health Initiative threw a wrench in the story, sending women in the opposite direction. The reluctance of women to take traditional hormone therapy left the door wide open for alternatives.
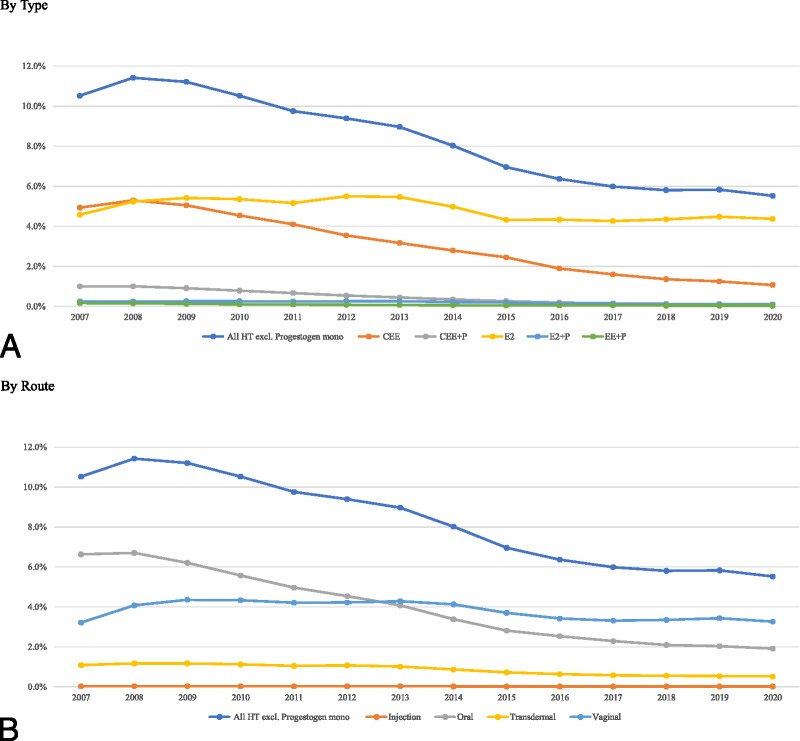
This is when bioidentical hormones became popular, also called bioidentical hormone therapy (BHT). Proponents say that it’s safer because the hormone’s structure is the same as what’s made in the body. And over time, more FDA options became available, and it's now the preferred treatment – transdermal estradiol and micronized progesterone over Premarin, conjugated estrogens (CEE) and progestins.
But now we’re seeing the pendulum swing once again, where women are made to feel guilty if they don’t take hormone therapy. I saw a respected medical doctor say on Instagram that estrogen is "the elixir of health for midlife women."
But what does the research really say?
A mix of benefits and risks
We know estrogen helps manage menopause symptoms like hot flashes/night sweats and prevents bone loss (while taking it) and in younger women; it has been shown to reduce the risk of diabetes, heart disease, and mortality.
Women under 60 and within 10 years of menopause mainly experience this effect, and the risk, although minimal, increases with age. Yet recent RCT trials like the KEEPS trial show a neutral effect in women who take MHT in 14 year follow up.
A 2021 umbrella review which is a review of review studies showed both benefit and risk to hormone therapy in both estrogen-only (ET) and estrogen plus progestogen therapy (EPT) in perimenopause and post menopause.
In the randomized control studies, MHT reduced vasomotor symptoms, fracture risk, vaginal atrophy (vaginal Et), sexual function, diabetes, cardiovascular mortality (ET) and colorectal cancer but increased the risk of stroke and venous thromboembolism, cardiovascular disease incidence and recurrence, deep vein thrombosis and lung cancer mortality (EPT).
Meta-analyses of observational studies linked MHT to decreased risks of cataract, glioma, and esophageal, gastric, and colorectal cancer, but increased risks of pulmonary embolism, cholelithiasis, asthma, meningioma, and thyroid, breast, and ovarian cancer.
A big shortcoming of this umbrella review is it did not decipher age, different MHT types, and lifestyle factors.
But a recent study looking at those who continued hormone therapy past 65 did separate by hormone type. And it gave us more insight.
Long-term use of MHT separated by dose and type
In 2022, The Menopause Society made a change in their position on the use of MHT in women 65 years and older, proposing that the decision should be individualized instead of stopping it. A recent study explored the effects of 40 different hormone preparation on 13 health outcomes in women who continued MHT beyond 65.
Here’s what most were taking:
Estrogen only (ET) was linked to 19% reduction in mortality compared to those without ET use. All combinations, routes, and doses showed reduction.
When separated out by route, vaginal ET, transdermal ET, and oral ET showed a reduction of 30%, 20%, and 11% respectively. It’s important to note that estrogen only (ET) both transdermal and oral is typically given to women without a uterus.
Estrogen plus progestogen had a neutral effect on mortality.
ET use was also linked to a 16% reduction in breast cancer. When looking at type CEE (23%) had a bigger effect than estradiol (12%). The WHI 13-year postintervention study showed a 23% decrease in breast cancer among women on ET.
When they looked at estrogen plus progestogen (EPT), there was a 19% increased risk of breast cancer. Separated out by type estrogen plus progestin was 20% and estrogen plus progesterone 10%. Lower doses had less of a risk of breast cancer.
As for other cancers, ET showed a 13% and 12% reduction in lung and colorectal cancer risk, while EPT showed a neutral effect. Only EPT with progestin decreased endometrial cancer risk (45%), EPT with progesterone increased the risk by 33%.
Ischemic heart disease showed a 4% increase associated with ET. Yet a low dose showed a tiny reduction of 1-2%. EPT (progestin) showed a 5% reduction whereas EPT (progesterone) had a null effect. For heart failure, ET showed reduced risk of 5% but a high dose increased it 5-17%. EPT demonstrated reductions of 4-5%, mostly associated with EPT (progestin).
ET use had no association or small reductions in stroke and dementia. Transdermal and vaginal estrogen preparations showed small (<10%) reduced risk. Yet a high dose ET increased the risk of both of these conditions by 8 and 3%. EPT had no associations, yet a low dose showed reductions.
Thoughts??
There’s a lot to take in here, but overall, this latest study shows minimal risk in continuing MHT past 65. The research assumes that many in this study started MHT earlier and continued. This differs from women who start over the age of 60 or 10 years past menopause.
ET alone seems to have a reduced risk of breast cancer. Because this is women without a uterus (and potentially no ovaries), I wonder if something else is going on. Or it really is the mixture of both estrogen and progesterone–not estrogen alone - that increases this risk.
It’s common to hear advice to women who don’t have a uterus to add progesterone anyway. But when you look at this evidence, I’m not sure that’s a good idea. Also, there were some benefits with the progestins over progesterone, except for breast cancer.
With age, lower doses of estrogen fare better in all categories of outcomes. But I see nothing that overwhelmingly benefits from taking hormone therapy if you don’t have symptoms. They don’t take into account lifestyle habits such as nutrition, exercise, etc., which likely plays a big role.
Also, vaginal estrogen was linked to lower mortality. I wonder if that’s because of the lower risk of UTIs which can be deadly as we get older, or if it’s just a fluke or healthy user bias.
The healthy cell bias
It’s important to note that estrogen can have both beneficial and not-so beneficial effects on the body. In a review entitled The necessary evil for human health, and how to tame it, Patel et al explain these dual roles:
The same estrogen ligands when bound to different receptors, exert different physiological functions by autocrine or paracrine mechanisms, of which some are beneficial for the body, and some are detrimental.
A lot of this has to do with what is called the healthy cell bias. Meaning in a healthy body, estrogen typically has positive effects, but in an unhealthy body, the opposite. Inflammation can increase the enzyme aromatase, leading to the overproduction of estrogen and negative effects. Yet too low levels of estrogen also can cause problems.
The hidden gem paper I talked about early this year is another potential answer to how estrogen can go bad. In women with compromised microvascular function, high levels of estrogen can make it worse.
In short, this paper says that “Homeostasis can be maintained by a healthy, personalized lifestyle.”
The missing pieces
It’s sad to see the reaction of older women after social media posts like the one I mentioned that makes them feel like they're missing out by not taking estrogen.
“Is it too late for me?” they ask.
What I want to tell them is that estrogen is one of many tools and as you get ten years past menopause, the other tools are a better choice. My research journey has taught me that keeping The One Health Principle from being disrupted is key.
Whether I go on estrogen, taking care of my body is paramount. Especially the fine tuning I’ve talked about and will continue to.
I know some women simply feel better on MHT and get health benefits while others don’t.
Yet something I’ve called the Vagina Problem remains and I encourage all perimenopausal/postmenopausal women to seek treatment, whether that’s vaginal estrogen, vaginal DHEA, or the medication Ospemifene.
I’ll keep you posted on my decision. Recently I went for a mammogram and the nurse asked if I was on estrogen. I said, “vaginal estrogen only.” And she said, “so you are on estrogen.” And I replied, “vaginal estrogen is not systemic.”
Later when I got my report, it said “On estrogen since 2023.” And I realize we still have a long way to go.
What decision have you made about hormone therapy? Share it in the comments.




Yes to estrogen plus progesterone plus vaginal estrogen. After essentially 5 years without stringing together two restful nights of sleep, the hormones are a game changer. I also share the vaginal estrogen with the thinner skinned areas of my face a couple of times a week. Thank you for a data-based, nuanced discussion of MHT backed up with studies.
I’m on all the HRT, including testosterone, coming up to three years now. I had all the symptoms and was not coping with them well at all. Now I have no symptoms and life is great.
That doesn’t mean I think everyone should rush out and get on HRT though. It’s such an individual thing and we are all different. What we do need to do is know what we’re talking about, and balanced posts like this one contribute towards that, thank you!
One thing I think often gets overlooked is that you have to be super consistent about taking HRT. So if you’re a person who doesn’t do well remembering to take medication for example, you might not do too well with some kinds of HRT either (e.g. gels you have to apply every morning). I haven’t heard that addressed anywhere yet.