
As I entered my 40s, I noticed my periods were heavier than usual. It was sort of subtle. Instead of one heavy day, it extended to two.
Then at 49, I spotted around the time I’d usually ovulate. Hmmmm. I mentioned this to my doctor, and they tested my hormones to inform me I wasn’t in perimenopause.
This is just my take, but the medical field didn’t seem to understand changes to the menstrual cycle in women over 40.
Now that I’m older, I’d like to help guide my younger friends about changes to the menstrual cycle after 40, as well as better understand my current stage.
Here’s what women over 40 need to know: Invariably there is a shift whether it’s in-between cycle bleeding, longer or shorter periods, and heavier flow.
This happens long before a skipped period.
Many women at this stage (like I did) go to their doctors and get their hormones tested, only to be told they aren’t in perimenopause.
But there’s the thing. Blood tests are not used to pinpoint where a woman is in the menopause transition. But menstrual bleeding is!
While much remains unknown about normal and abnormal menstrual bleeding after age 40, I’ve compiled the available evidence to help women understand what to expect.
Stage 1: The late reproductive years or “very early perimenopause”
A big part of the problem is the medical community doesn’t recognize the early stages of the menopause transition, when cycles are regular, and women are younger.
Researchers often exclude women in their 40s from research studies on the menstrual cycle. Yet a first-of-its kind large 2024 study aimed to solve that by using a popular app.
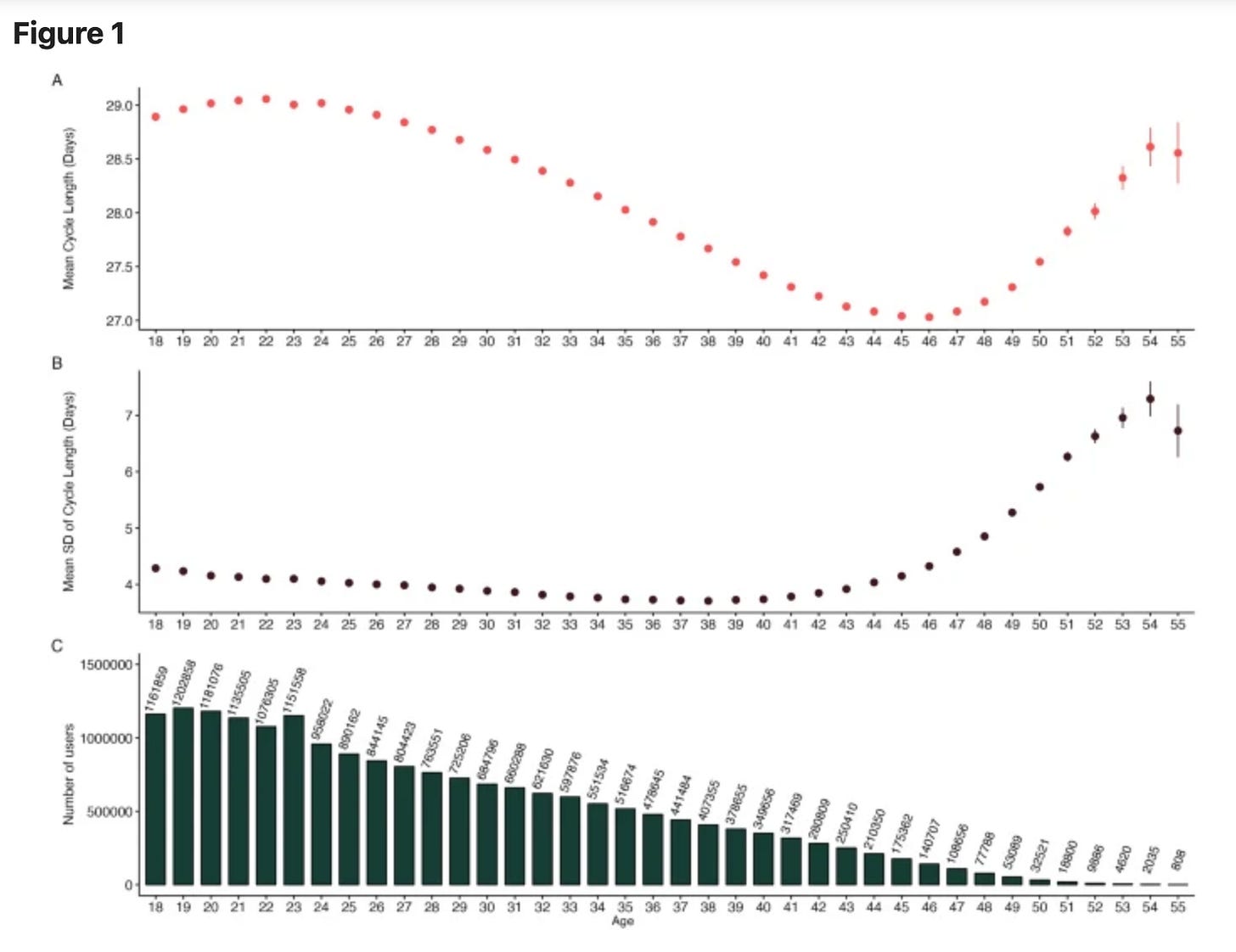
The study included over 19 million women aged 18-55 over a 12-month period using the Flo app.
They found that cycle length shortens from 28.54 days in the 18-25 group but decreases to 27 days in the 40s. Yet cycle length increases again after age 45.
Actual periods were longest in the 18–25 age group, with a mean duration of 5.20 days compared to 5.06 in the 40-45 age group.
Heavy bleeding is common. About a third of women 40-45 years of age experience regular heavy menstrual bleeding, two-thirds of women 40-54 have experienced heavy bleeding in the last six months.
How hormonal changes affect your cycle
Women in this stage tend to have higher levels of estrogen as their body aims to use up the remaining eggs. Because estrogen builds up the uterine lining, periods can become heavier.
There also may not be enough progesterone to counteract the effects of these higher levels of estrogen. And after 45, anovulatory cycles increase, meaning progesterone is lower.
Yet non-hormonal issues need to be checked out because they can cause heavy bleeding.
When it’s not normal
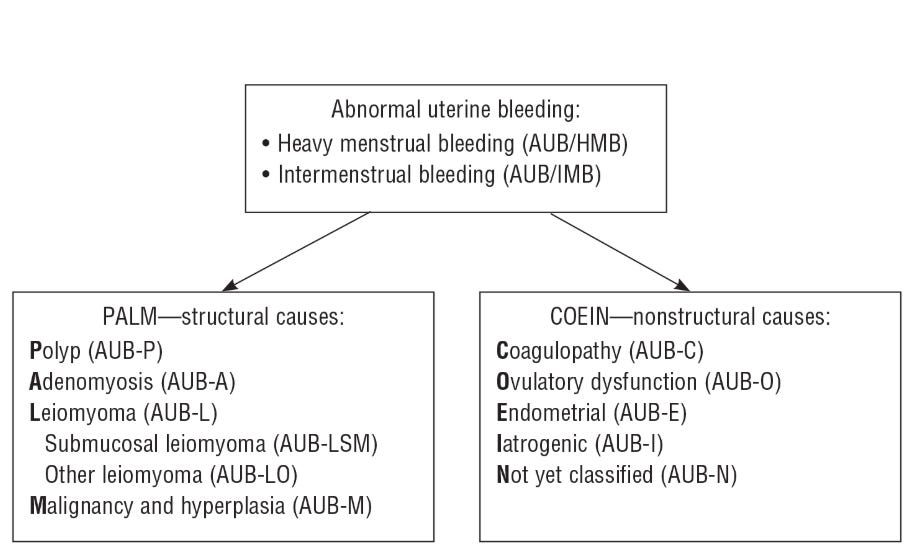
The American College of Obstetricians of Gynecologists (ACOG) defines abnormal uterine bleeding (AUB) as:
Bleeding from the uterine corpus that is abnormal in its regularity, volume, frequency or duration and is not associated with pregnancy.
In premenopausal women, bleeding issues can be due to structural such as polyps or fibroids or nonstructural causes like ovulatory disorders. Clinicians refer to this as PALM-COEIN.
In short: although hormonal fluctuations during this stage can cause heavy and breakthrough bleeding, structural issues like polyps and fibroids, which increase with age, can also cause it.
In fact, the highest incidence of polyps is between the ages of 40-44.
What to do?
It’s a great time to get regular physicals and check those biomarkers. Specifically, heavy menstrual bleeding often causes iron deficiency in women, and low vitamin D is linked to fibroid growth.
Although malignancy is uncommon at this stage, it’s a good time to get checked out.
This is the perfect time to move over to a menopause specialist instead of a regular OBGYN. Some women may do well on progesterone at this phase, so bring that up—along with other options - with your specialist.
In younger women, talk about testing to rule out if any bleeding changes are because of hormones. Anti-Mullerian hormone (AMH) can estimate egg reserve and FSH levels can give more information on impending menopause.
“Not once has my doctor said the word perimenopause as a factor in my bleeding changes,” said Holly, aged 45. “I just think after all these tests came out normal, it really is about my hormones.”
Stage 2: Perimenopause
The STRAW staging system defines early perimenopause as a change in menstrual cycle length of 7 days or more.
Most have short (<21 days) or long (>36 days) cycles that are increasingly anovulatory, which means there’s no progesterone activity. In this phase, erratic bleeding is common.
In one study with 1320 midlife women, three out of four experienced at least three episodes of 10+ days of bleeding. Periods followed by spotting occurred in over half of them.
And periods with heavy bleeding for three or more days occurred in one out of three, with 40% experiencing heavy bleeding three times in 6 months.
Late menopause is once a woman goes over 60 days without a period. This is a time bleeding calms down, although random heavy periods can still occur.
In short: periods get whacky first and eventually you’ll go longer between bleeding sessions.
How hormone changes affect your cycle
With anovulatory cycles on the rise >45 years of age, women can expect to see more spotting and sporadic, heavy bleeding. After all, estrogen thickens the lining while progesterone thins it.
Where there’s bleeding, there’s estrogen.
About 5 years before the last period, progesterone decreases, but estrogen doesn’t decrease until two years before.
Once a woman goes over 60 days without a period (late peri) estrogen is on the decline.
When it’s not normal
I was happy to find a review that defines “perimenopausal AUB”, although it’s quite vague:
any abnormal menstrual bleeding during menopausal transition or within the first year after menopause (except for cyclic bleeding in women using hormonal replacement therapy)
Over 90% of perimenopausal women have AUB and 78% have it at least three times as they transition through menopause.
Similar to the previous section, ruling out causes is important. Most doctors do this by performing a hysteroscopy, which is when they insert a thin, lighted telescope-like devise into the uterus to look around.
At this stage, endometrial polyps and fibroids are still the most common causes of structural bleeding issues.
When I was in early perimenopause, they found a polyp, and I had it removed. Although I had some bleeding after, it gradually lightened up. But I’m not sure if it was the removal of the polyp or me just heading to the next stage: menopause.
What to do?
Same as above—get regular physicals and get those biomarkers checked. Women are still at risk of iron deficiency and low vitamin D is linked with the growth of fibroids.
With any bleeding issues, one must rule out malignancy, although it is still uncommon.
If you haven’t already, move over to a menopause specialist instead of a regular OBGYN. Some women may do well on progesterone in early perimenopause, while estrogen may be an option in later peri. Discuss options with your specialist.
Stage 3: Menopause
One year without a period defines menopause. But how do we define a period?
During my wait for menopause, I had the classic signs of ovulation. About two weeks later, I experienced some spotting, which made me think my period was coming.
But it never did. Did the spotting I had count as a period? I didn’t think so.
So, I didn’t count it and considered that my body’s last hurrah. Only it happened again a couple of months ago with even more spotting.
We need clearer guidelines on super light bleeding that can happen at the very end of the transition.
However, postmenopausal bleeding always warrants a medical examination.
it is possible a spontaneous ovulation occurs post menopause like in this 57-year-old women three years post menopause, but that is rare.
Women with bleeding post menopause have a higher risk (21%) of endometrial cancer or atypical hyperplasia, so you want to get checked out.
Other causes of post-menopausal bleeding (PMB) include vaginal/endometrial atrophy, infections, medication, polyps and genitourinary atrophy.
How hormone changes affect your cycle
Now that blood hormone levels are low, bleeding stops. The body makes estrogen intracellularly but doesn’t release it into the bloodstream. This is important to not stimulate growth in the endometrial lining.
When it’s not normal
in postmenopausal women, doctors often check the thickness of the endometrial lining with a transvaginal ultrasonography.
If the linking is equal to or less to 4 mm, there is a greater than 99% chance a woman doesn’t have endometrial cancer.
If bleeding continues, there could be other non-genitourinary reasons for the bleeding.
What to do?
This is a good time to discuss options for hormone therapy in this post menopause period
Vaginal estrogen (or other non-hormonal options you can speak to your doctor about) can be lifesaver not only for genitourinary symptoms but reducing risk of UTIs and vaginal atrophy.
No periods because of birth control
Women on birth control in their 40s and 50s, such as the IUD or oral contraceptive pill, will not know what stage they are in. Women can work with a menopause specialist in testing and tracking symptoms.
And planning when to safely stop using birth control.
Summary
Starting in our 40s, bleeding patterns change first subtly and then not-so-subtle.
Mainstream doctors who aren’t familiar with the menopause transition will often test hormones instead of looking at bleeding patterns. They can also make women undergo unnecessary tests and treatments.
Do yourself a favor and find a specialist such as a doctor certified by the Menopause Society.
We need more research to better define bleeding after 40. But for now, just know changing hormones = changing bleeding patterns.
Aging also increases the risk of polyps and fibroids complicating matters; and we always want to rule out cancer.
Let me know how bleeding has gone for you in the midlife stage!
Information in this post is meant to educate and not replace medical advice. Talk it over with your healthcare provider!




At 40, my periods were heavy, long cycles and endometriosis flared as well, which makes sense because estrogen was dominating the show and progesterone was falling flat.
It took years, but now at 45, I've been on progesterone cream for about 3 years and incorporated DIM/CDG to help clear out excess circulating estrogen.
I've incorporated other practices like, cycle awareness (of course ;-)), changing my lifestyle to go with my cycles instead of forcing my cycles to fit the grind of life.
My cycles went from irratic 28-35 days (mostly the latter) to now 27-31 days and the flow is now much much lighter, yet a bit wobbly. My endo pain has been gone at my 1 year anniversary of pain free with only mild cramps for 1 day.
I feel like my cycle is the healthiest its been in decades, but the perimenopause symptoms are I guess not to be avoided. LOL
It is an untethering like nothing I've ever known.
Maryann, thanks for another great article. Be sure to put this in The Women's Health Collective 365!
Great summary of the changes to expect. My cycle followed the shorter then longer pattern as well. Very happy to be comfortably settled in post-menopause now!