
At age 43, during a routine physical, I asked my doctor for advice on what I should be doing now that I was in my 40s.
“You’re already doing it,” she said.
At the time, I was taking vitamin D and exercising regularly. I didn’t think much of her response, but looking back, I realize she was implying that my needs weren’t changing—when in fact, they were. I would go through a lot before I figured that out.
This is why I have mixed feelings about October, which is Menopause Awareness Month. While we’ve made significant strides in raising awareness about menopause, we’ve made little to no progress in recognizing the broader challenges of midlife.
I see this as a major blind spot in the current menopause movement. Sometimes, I feel like I’m the only one waving the flag for midlife awareness.
So, as I reflect on that time in my early midlife, I want to share with you all the things I wish she had told me.
Your 40s mark the beginning of a new developmental stage
Okay, back to my question: What should I be doing differently now that I’m in my 40s? In my ideal world she would’ve said:
Your 40s mark the beginning of a new developmental stage, which extends from around age 40 to 65.
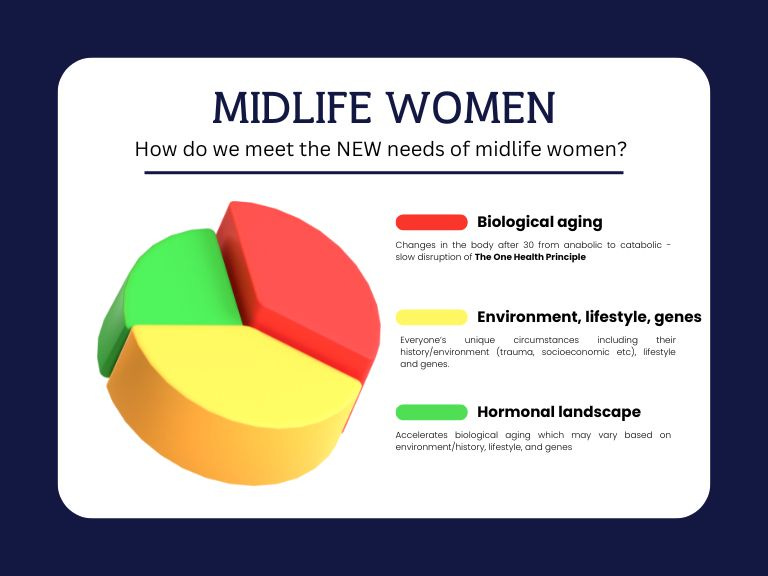
This is a time when the signs of biological aging start to appear, due to a physiological shift that begins after age 30. By the third decade of life, your body transitions from an anabolic (building) phase to a catabolic (breaking down) phase.
This means muscle mass and power start to decline. You are no longer building bone and may even start losing it, depending on your genetics, risk factors, and lifestyle.
After age 30, changes also occur in your autonomic nervous system. There is a gradual increase in sympathetic activity (fight or flight) and a decrease in parasympathetic activity (rest and digest). By the time you reach 40, these changes can manifest as irritability, mood swings, sleep disturbances, and anxiety.
READ: Meet Your New Post-40 Nervous System
These and other signs of biological aging can gradually increase inflammation and oxidative stress while decreasing nitric oxide, a vital signaling molecule that keeps your arteries flexible and prevents plaque from forming on the arterial walls.
This is part of what’s known as the "One Health Principle" — where inflammation and oxidative stress increase while nitric oxide decreases.
Endothelial cells, which line both large and small blood vessels, secrete the vasodilator nitric oxide. When nitric oxide levels decline, it can lead to endothelial dysfunction, which is the first step in the development of heart disease.
Be ready for hormonal changes
If you haven’t already, you’ll soon experience hormonal changes. The average age of natural menopause—defined as one year without a period—is around 50. This means that if you're average, perimenopause will probably start in your mid 40s.
Perimenopause is the transition period before menopause when menstrual cycles begin to wind down. It typically lasts 1–5 years, but can extend up to 10 years depending on how it’s defined. The start of this transition is determined by your ovarian reserve (the number of eggs you have) rather than your age.
Many women assume their hormones decline first, but during the late reproductive years, estrogen levels can actually be higher than usual before perimenopause.
At the same time that estrogen levels increase, progesterone levels may stay the same or even decline, which throws the body out of balance. Estrogen doesn’t decline until about two years before your final period, while progesterone typically drops about five years before.
In short, hormonal changes start happening just as women are already feeling the effects of biological aging, making it difficult to pinpoint what’s driving changes in how they feel.
That’s why it’s important to check everything: iron levels, vitamin B12, vitamin D, and thyroid function. Let’s do a full lab workup, get a baseline bone density scan, and go from there.
This sounds like heaven…to skip the years of fatigue and scary palpitations from my iron deficiency would have been a lifesaver!
Paige assumed her sore tongue, twitchy eye lid, and feeling off was due to perimenopause, but it was actually a B12 deficiency.
“Five years ago, I had low energy and was acting irrational (for me)” she said. “I thought I was just going through perimenopause and that's why I felt crazy, but I actually was low in Vitamin B12.”
And doctors diagnosed Rebekah with osteoporosis at age 28! Talk about a shocker, but a good thing she found out.
But back to the doc…
Now is the perfect time to make lifestyle changes that align with the changes happening in midlife.
However, some women are more vulnerable during this phase (often called the "Aging Pause"). This includes women with a history of trauma, anxiety, depression, hormonal sensitivity, or severe PMS.
Don’t delay getting the mental health support you need. It’s also a good time to talk to your mother or other relatives about their menopause experience, as genetics can play a significant role in your experience.
READ: Investing in Emotional Health at Midlife
Menopause: the accelerator
Of course, this covers early midlife, but that’s the point. Most women entering midlife are still about 10 years away from menopause. That’s one reason it’s a mistake to make midlife only about menopause.
I’m fortunate to be approaching late menopause, and as things stand, I will likely reach it at 55 (next month). I believe that addressing my changing needs has helped ease the hormonal shifts, which work to speed up what is already going on.
Women in menopause or postmenopause need to understand that when sex hormones decline, menopausal hormone therapy (MHT) is an option to relieve symptoms and prevent bone loss. Earlier on, and even once menopause begins, progesterone alone may be helpful.
But that’s just one part of the picture.
With "Aging Pause," women need to be aware of the risk of several micronutrient deficiencies, including choline, vitamin D, vitamin B12, magnesium, and the long-chain omega-3 fatty acid DHA you can read more about here.
Many of the “symptoms” during perimenopause and menopause—especially hot flashes and sleep disturbances—are not benign. They can be signs of that pesky endothelial dysfunction that can start in early midlife.
Since both estrogen and progesterone stimulate the release of nitric oxide—which already declines with age—menopausal women are hit hard.
To complicate matters further, there are connections between endothelial dysfunction and bone loss, insulin resistance, and losing lean body mass.
READ: To Take Hormone Therapy or Not to Take Hormone therapy
It's time to take off our blinders
Leaving midlife unexamined is a major blind spot in women’s health. Not only have we been overly focused on hormonal changes, but mainstream support for midlife women tends to prioritize relieving vasomotor symptoms with hormone therapy or medications like antidepressants or the new Veozah - just one part of the pie.
However, if we know these symptoms are linked to poor metabolic health, why aren't we prioritizing nutrition and lifestyle interventions that address both biological and hormonal changes?
How is it possible that we still don’t have a marker for endothelial dysfunction, the pre-heart disease risk factor that’s connected to almost every major health issue midlife women face?
Although midlife is the bridge between young adulthood and older age, we’ve done so little to understand this life stage beyond hormones.
A 2022 review study published in the Journal of Women’s Health found that midlife and menopause receives the least amount of research attention compared to pregnancy, and postmenopause (older age).
Through this Substack, I’m doing my part to help define the needs of midlife women, including posts and interviews with experts who are doing innovative work and research.
Change is way overdue
It’s time we approached midlife the same way we approach other developmental stages.
These stages, such as infancy, childhood, and old age, have dedicated journals, societies, and tailored recommendations to maximize health during that phase of life.
As Margie Lachman, a psychologist and expert in lifespan development, wrote in the 2015 journal Research in Human Development: “It’s fair to say that of all the periods in the life course, the middle years, roughly ages 40 to 59, are the most overlooked. There are no journals or professional societies specifically devoted to midlife, yet all other age periods—infancy, childhood, adolescence, young adulthood, and old age—have dedicated publications and organizations.”
Last time I checked, there was only one midlife health journal and one professional society.
It’s time to change that. Let’s bring midlife into the spotlight and ensure our needs are recognized! Join the movement to raise awareness and advocate for the well-being of midlife women everywhere.
Share this post, send to a friend, restack it, or simply press the heart. And let’s talk more in the comments.




Great post! It feels to me like the big disconnect is between all the possible symptoms related to peri and menopause and the timing. Most women have no clue they can start as early as they do. If I had known then what I know now, I would have been looking out for symptoms, testing sooner and treating them much earlier.
An excellent article thank you. A recent visit to my male gynae, I mentioned the aches and pains I am experiencing and questioned whether they were signs of peri menopause and he replied that he got them too and was certainly not in menopause!! It was a good reminder of aging-pause. I believe so much work needs to be done in women's health (exclusive of men) but sometimes a few reminders that our experiences are across the board would be so helpful too.